Pandemics occur when an epidemic spreads widely enough to encompass the world (or at least a very large portion of it).
They could also occur when a new strain of virus emerges for which people have no previous exposure. Although medical advances and population characteristics have substantially improved the ability of epidemiologists and health care providers to cope with pandemics, they can still strike with unpredictable severity.
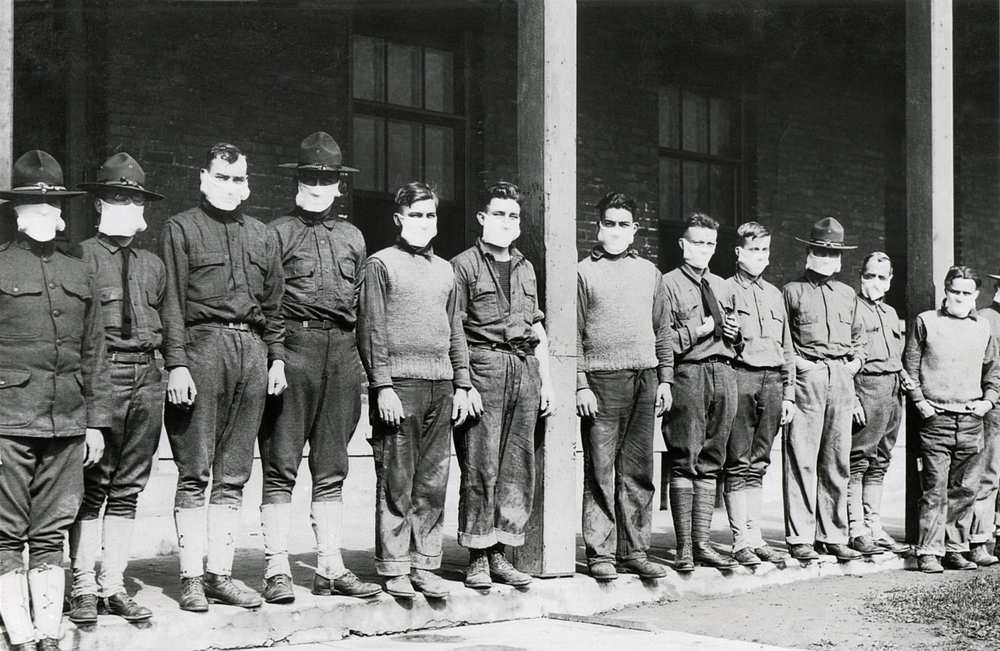
Think of the Spanish Flu, which emerged a century ago. It was possibly the most significant pandemic in human history and an epidemiological event still unparalleled in geographic reach, infectiousness, and virulence (severity). Spanish Flu spread rapidly throughout the world, killed with remarkable swiftness, and had strong staying power. All told, an estimated 50 million people worldwide died during its unusually long 18-month cycle.
Although influenza is not feared nearly as much today as it was 100 years ago, due to more effective medical and non-pharmaceutical interventions and better health care, non-seasonal influenza still poses high pandemic risk.
Pandemic influenzas can be characterized by rapid and frequent mutation, high human-to-human transmissibility, and variable virulence. Although prior exposure, especially early in life, can partially mitigate severity, the virus’s high mutability has meant continued population vulnerability.
Indeed, the H1N1 virus, which caused Spanish Flu, has been a factor in several large-scale influenza outbreaks – most recently in 2009’s Novel A/H1N1 Swine Flu pandemic. And H3N2, the fast-mutating culprit behind this year’s seasonal flu epidemic, is causing the
current flu season to quickly approach 2009’s in population impact. Indeed, by mid-February 2018 – more than midway through the current Northern Hemisphere flu season – cases have been reported throughout the U.S. and in Puerto Rico, and more than 60 pediatric deaths have been recorded as of this writing.
Efforts to create a universal flu vaccine (against pandemic and seasonal influenza), although theoretically promising, have thus far not been successful. Seasonal vaccines are effective, but their effectiveness can vary from season to season. Consider that in 2014-2015, the vaccine covered only 23% of that year’s circulating viruses. The vaccine for this year’s flu season, currently in full swing, is projected at approximately 25% effectiveness for H3N2, the dominant circulating U.S. strain.
What might the next pandemic look like? Factors such as antibiotic resistance, a constant stream of emerging pathogens and mutating viruses, a still-developing understanding of how viruses and other pathogens evolve, and external factors such as the potential impact of bioterrorism make it difficult to conclusively predict when the next one might strike and what its impact might be.
Notwithstanding their unpredictability, populations can be protected against the possibility of a pandemic and the impact of an outbreak mitigated. Factors today that might predict a less-severe impact from pandemic include:
- The speed at which a new pathogen can be identified and studied including use of artificial intelligence and machine learning
- The ability of governments to establish precautionary measures (e.g., quarantines, curfews)
- Instantaneous global communication sharing information as gathered
- Antivirals to treat influenza itself and antibiotics to treat complications such as pneumonia
- Better general population health compared to a century ago
Currently, there is no single model for assessing infectious disease pandemic risk. The three best-known university-developed models – The Imperial College Model, University of Washington Model, and Virginia Bioinformatics Institute Model – as well as others developed by specialized private companies, all primarily base their calculations upon Spanish Flu experience and data. The emergence of the highly pathogenic H5N1 strain in 1997, the H7N9 strain in 2013, and the re-emergence of H1N1 in 2009 have increased the insurance industry’s need for stronger and more precise pandemic modeling.
In general, most frameworks assessing the severity risk of the next pandemic weigh the favorable aspects of modern times more heavily than the unfavorable aspects. However, to fully assess the potential pandemic mortality tail risk in extreme events, insurers must understand the factors or inputs to the various model methodologies.