The most recent version of the International Classification of Diseases, 11th Revision (ICD-11), is introducing a new paradigm regarding the classification of pain.
This novel approach stratifies pain in ways which are unprecedented and will be new to many readers. It will be critical for insurance medicine professionals to understand these concepts as they will likely impact the assessment of risk and may even affect how claims are assessed and adjudicated.
This is Part I of a two-part article that will explore the new pain nosology. Part I will focus primarily on discussing chronic pain in general as well as chronic primary pain syndromes. Part II will address chronic secondary pain syndromes.
Background
To date, the International Classification of Diseases (ICD) has not provided systematic representation of chronic pain states. The only formal systematic categorization of pain syndromes has been that of the International Association for the Study of Pain (IASP). The most recent (second) edition of that nosology (classification of diseases) was released in 1994 and updated in 2012.1 A perceived shortfall of appropriate coding was seen as contributing to the inadequacy of evidence-based treatment pathways for persons with persistent pain states.
A new classification system for chronic pain has now been developed by an interdisciplinary task force convened by the IASP in consultation with the World Health Organization (WHO). This new diagnostic system distinguishes chronic primary and chronic secondary pain disorders, integrates existing diagnoses, and claims to provide precise definitions consistent with the content model of the ICD. Released by WHO in June 2018, ICD-112 is expected to incorporate this new classification of pain states soon; the decision to do so may be voted on as early as May 2019.
As occurs wherever a new classificatory system is launched, this new nosology is heralded as being “clearly operationalized and easily measurable.”3 Among the stated aims of this new system is the hope that in the future, clinicians and others will be aware that pain can present as the dominant or even sole medical adversity experienced by an individual.
The task force reminds us that while persistent pain may be secondary to an underlying disease process, it frequently persists beyond the normal healing process despite there being no other identifiable explanation. This new classification framework provides a system of suitable diagnoses for pain conditions irrespective of the temporal relationship to other somatic morbidities, be they resolved or ongoing morbidities, or indeed when no associated physical disorder has been identifiable.
Complicating the landscape, a focus of this new nosology is to de-emphasize psychiatric constructs pertaining to somatoform presentations and disorders, resulting in some discordance with past and current (2013) versions of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM).
The interdisciplinary task force has provided an overview document1 and several related co-published articles detailing these proposed diagnoses. In the introduction to their article on Chronic Primary Pain,4 authors M.K. Nicholas and team indicated dissatisfaction with the definitions and descriptions in the current ICD and DSM, stating that “both have been found wanting in their accounts of chronic pain conditions … neither system reflects the developments in pain research over the last two decades and they do not have clear treatment or management implications.”
The German-language version of ICD-10 employed diagnostic language for complex pain presentations which was widely considered most appropriate of all: “chronic pain disorder with somatic and psychological factors.”4 While this language acknowledged potentially equal causal attribution to psyche (mind) and soma (body), concern has been expressed that the chronic pain diagnosis continues to be categorized in the psychiatric section.
Appropriately, pointing to advances pertaining to the established science underpinning psychological, social, and central nervous system mechanisms, the authors opined that classifications of chronic pain presentations must accommodate the multiple interacting contributors and set aside considerations of somatic versus psychogenic. They even go so far as to state that a dichotomized consideration such as this has become obsolete given medicine’s advancing neuroscientific insights.4 Such opinions are laudably sophisticated, yet are by no means novel within the psychosomatic medicine fraternity.
Pre-empting the concern that this diagnostic system minimizes or even rejects the potential role which can be played by psychogenesis, Nicholas et al. do acknowledge that “biological changes are closely linked to psychological processes; this is most obvious in neurophysiological brain reactions contributing to changes in pain perception.”4 The reader should appreciate the established knowledge that both pain and mood/anxiety are processed by multiple overlapping parts of the brain’s limbic system (i.e., the collected areas pivotal to the regulation of mood, arousal, anger, and impulse), and that this set of shared neuropsychiatric components is widely considered pertinent to aspects of a bi-directional causality apparent in these conditions.
The interdisciplinary panel brought together by the IASP to establish this new classificatory system noted that the novel proposed categories could assist in reducing stigma attached to chronic pain syndromes. To quote: “Because of the success of the behavioral neurosciences, even mental disorders can nowadays no longer be considered purely non-somatic. Of note, all chronic pain, including chronic primary pain, will be coded specifically outside the realms of psychiatric disorders. This accords more with the current scientific understanding of chronic pain and often aligns better with a patient’s own views.”2
As a curious aside, and cognizant again of advances in neuroscience, by the same reasoning one might reasonably suggest that conditions such as schizophrenia and bipolar disorder too cannot be categorized as purely non-somatic; rather, these too are becoming recognized as integrated biopsychosocial phenomena, with increasingly well- defined neuropathological underpinnings. This arbitrary separation of all pain states from familiar historical psychiatric categorizations might warrant some further consideration.
The following is a discussion of the new chronic pain diagnoses and how they are designed to be applied once integrated into ICD-11.
Overview
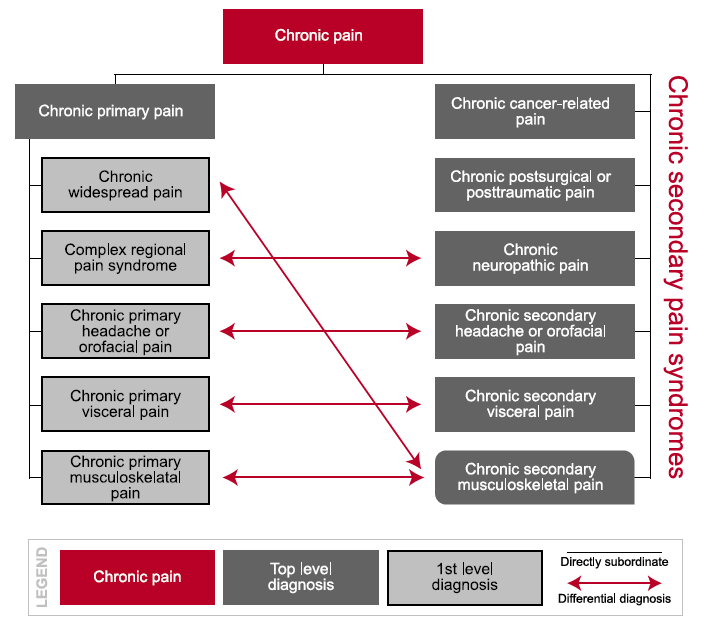
First, chronic pain is a parent code for seven other top-level diagnostic codes dealing with more common, clinically relevant types of chronic pain conditions:
• chronic primary pain
• chronic cancer-related pain
• chronic postsurgical or post-traumatic pain
• chronic neuropathic pain
• chronic secondary headache or orofacial pain
• chronic secondary visceral pain
• chronic secondary musculoskeletal pain
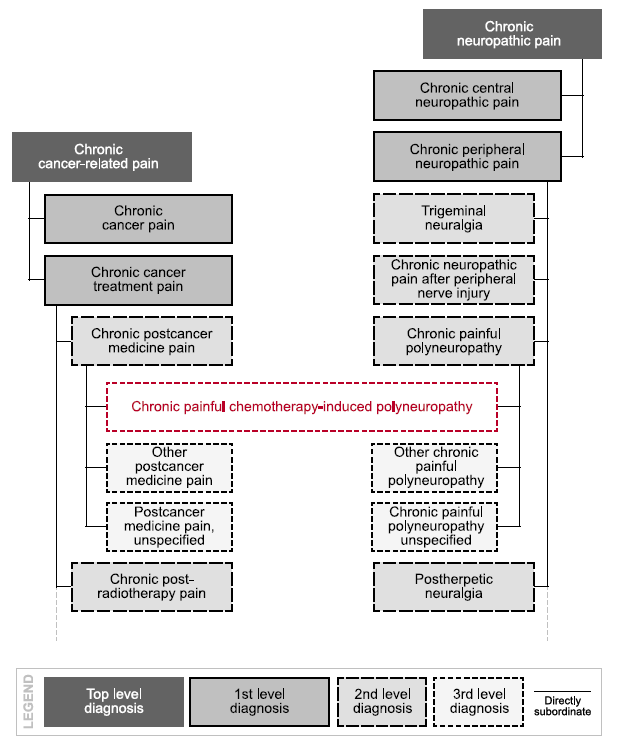
Figure 1, below, provides a representation of the relationship between this parent code and the above top-level diagnoses, as well as some first-level diagnoses. In chronic primary pain syndromes, as detailed on the left, pain itself is seen as a disease in its own right, whereas in chronic secondary pain syndromes, detailed on the right of the diagram, pain initially manifests as a symptom of some other impairment process, such as cancer, accident, nerve damage, or inflammatory disorders.
Figure 1:
Hierarchy of Chronic Pain Diagnoses
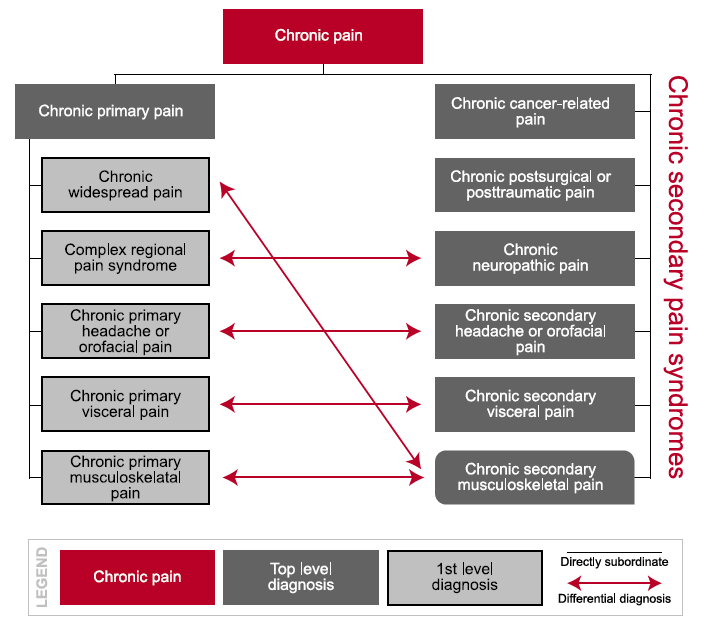
Source: Adapted from Treede RD, et al. Chronic pain as a symptom or a disease: The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain. 2019 Jan.
A differential diagnosis between primary and secondary pain conditions can sometimes prove challenging. Still, in either case, a person’s pain warrants appropriate attention in accordance with the degree of severity and related impairments.
After a spontaneous healing or successful management of an underlying pathological process, persistent pain may sometimes continue and hence the chronic secondary pain diagnosis may remain.
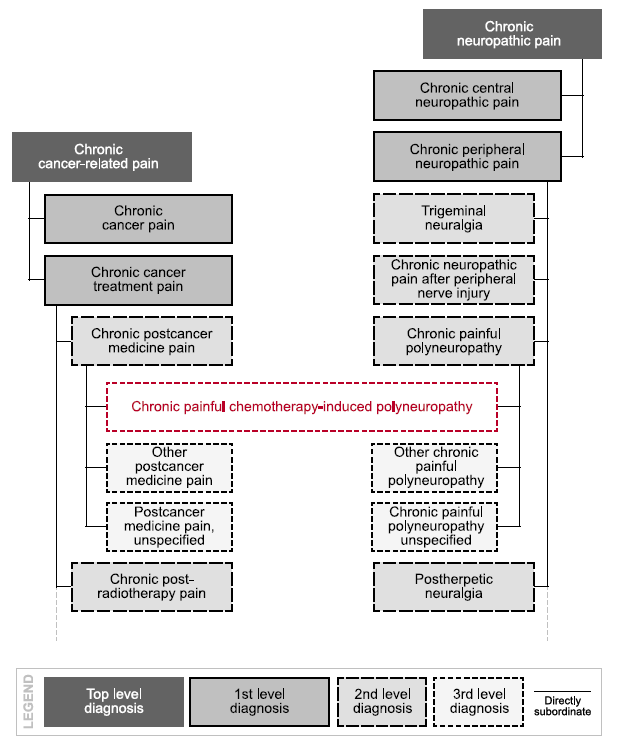
There can be some overlap between these pain conditions; for example, neuropathic pain caused by cancer or its treatment. There can also be overlap between these pain definitions and other disorders in the ICD such as persistent headaches. ICD-11 addresses this by allowing what it calls “multiple parenting,” as shown in Figure 2.
Figure 2:
Multiple Parenting Construct for Pain
Source: Adapted from Treede RD, et al. Chronic pain as a symptom or a disease: The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain. 2019 Jan.
Chronic Primary Pain Syndromes
Chronic primary pain is defined as “pain in one or more anatomical regions that persists or recurs for longer than three months and is associated with significant emotional distress or functional disability (interference with activities of daily life and participation in social roles) and cannot be better accounted for by another chronic pain condition.”2 This is a new category of disorders that apply to chronic pain syndromes not consistent with an identifiable pathology, and so are considered to be best conceptualized as disorders in their own right.
This classification category is specifically designed to detail poorly understood conditions without the application of the former “obscure and potentially laden terms such as somatoform, non-specific, or functional.”4 Some critics have protested that this new category unreasonably de-emphasizes psychiatric processes in such presentations. However, the interdisciplinary task force considered such concerns to be unreasonable and lacking in evidence.
In addition to neuropathic and nociceptive (relating to the perception or sensation of pain) phenomena integral to many primary (and secondary) pain disorders is the recently defined phenomenon of nociplastic pain. Nociplastic pain refers to a neurophysiological mechanism which causes pain to arise because of altered nociception, despite an absence of actual or threatened tissue damage causing neuronal activation, and absent any impact due to identifiable pathology of the somatosensory nervous system.5
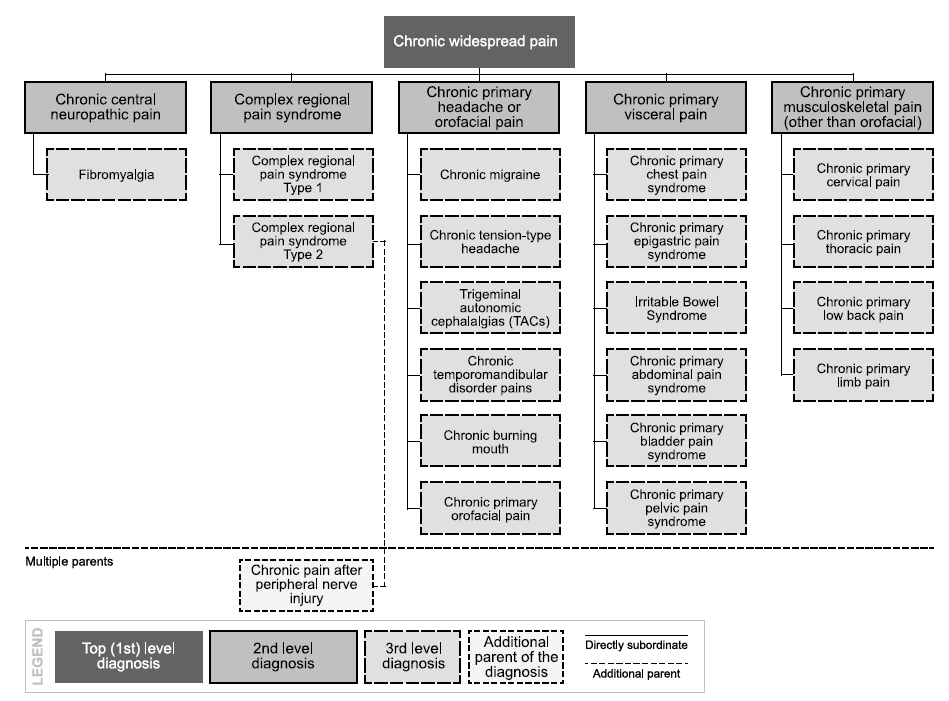
Figure 3:
General Classification Structure of the Hierarchy of Chronic Primary Pain
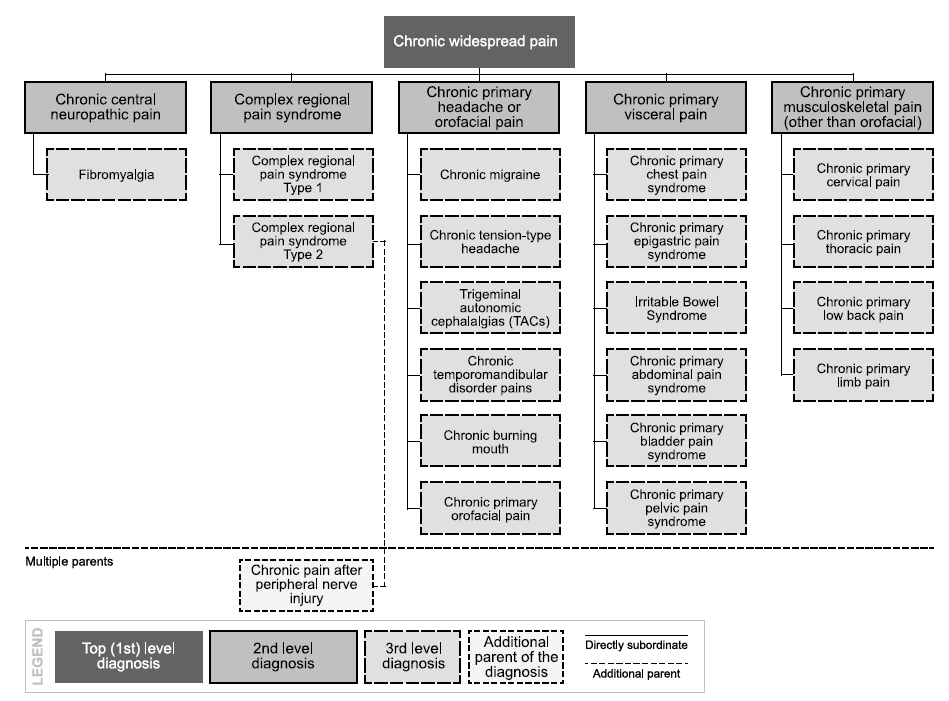
Source: Nicholas MK, et al. The IASP classification of chronic pain for ICD-11: chronic primary pain. Pain. 2019 Jan.
As indicated in Figure 3, the chronic primary pain classification is subdivided into the following:
chronic widespread pain (e.g., fibromyalgia)
complex regional pain syndrome
chronic primary headache and orofacial pain
chronic primary visceral pain (e.g., irritable bowel syndrome)
chronic primary musculoskeletal pain (e.g., non-specific low back pain)
Of course, symptom profiles adequately explained by identifiable pathology discount any of the above primary diagnoses. Chronic secondary pain syndromes must be considered and excluded where possible.
Chronic primary headaches will be cross-referenced, making use of the multiple parenting option of ICD-11. For example, chronic migraine is listed both in the headache session of ICD-11 and the chronic pain section.
Chronic Widespread Pain
Chronic widespread pain (CWP) is a diffuse experience perceived in at least four of the five specified body regions and in at least three or more body quadrants and axial sites. As a primary disorder, the pain is not attributable to an identified nociceptive process in these regions. There will be features consistent with nociplastic pain, such as sensory derangements including spontaneous or excessively evoked pain
in the affected regions, and there will be identifiable psychological and social factors contributing to the presentation. Comorbid disturbances will be common as well.
Fibromyalgia syndrome (FMS) is an example of CWP. It is commonly associated with sleep disorders, cognitive dysfunction and other somatic complaints, including irritable bowel syndrome (IBS) and chronic fatigue syndrome.
Complex Regional Pain Syndrome
Complex regional pain syndrome (CRPS) has two types: CPRS type I and CPRS type II – and involves pain in a specific region, usually precipitated by trauma. The pain and/or its duration is markedly in excess to that which would be expected. CRPS is characterized additionally by signs and symptoms of autonomic and inflammatory change in the affected part. Symptoms may include hyperalgesia, allodynia (pain resulting from a stimulus which would not normally provoke pain), skin temperature change, perspiration, fluid retention, and altered hair and nail growth. Localized osteoporosis can often ensue.
Symptomatology may alter over time, most likely related to nociplastic mechanisms.
In CRPS type I there is no identifiable associated peripheral nerve injury, whereas in CRPS type II identifiable nerve injury is present. (A definition for CRPS can also be found in the ICD-11 section detailing disorders of the autonomic nervous system – another instance of the multiple parenting used in the ICD 11.)
Chronic Primary Headache and Orofacial Pain
These types of pain are defined as conditions that occur on at least 15 days per month and for longer than three months. The duration of symptoms each day is at least two hours when untreated. For many individuals, briefer episodes may occur daily. Other chronic head and orofacial conditions are listed under chronic secondary disorders:
- Chronic migraine is defined as in the prior paragraph, provided the presentation of the features are consistent with migraine headache. These include a generally unilateral pulsing pain of moderate to severe intensity. Migraine is commonly exacerbated by physical activity, and may be associated with nausea and/or aversion to light (photophobia) or sound.
- Chronic tension-type headache is defined as a frequent episodic headache, typically bilateral, with a pressing or tight quality. While these too may be associated with nausea, photophobia, or sensitivity to sound, they are not usually affected by physical activity.
- Trigeminal autonomic cephalalgias (TACs) involves unilateral facial or head pain, usually occurring along with significant local autonomic features such as lacrimation, rhinorrhoea, nasal congestion, and eyelid swelling. This category includes diagnoses of cluster headache and paroxysmal hemicrania.
- Chronic temporomandibular disorder (TMD) is one of the most common forms of persistent facial pain. It involves not only the temporomandibular joint (TMJ or jaw hinge) but also the muscles of chewing and related tissues. There are also forms of chronic secondary TMD.
- Chronic burning mouth is a distressing disorder which in some people is quite debilitating. Care must be taken to distinguish this from a secondary burning mouth syndrome, which might be attributable to infections or even in some (rare) cases vitamin D deficiency.
Chronic Primary Visceral Pain
Chronic primary visceral pain may be localized to the head or neck, thoracic, abdominal, or pelvic regions. Included in this category may be non-cardiac chest pain, centrally mediated abdominal pain syndrome, IBS, and chronic anal, pelvic, and testicular pain. Notably, a number of disorders formerly termed “functional,” psychogenic, or somatoform are now included among chronic primary visceral pain diagnoses and have attracted new names accordingly.
Also included in this diagnostic category is chronic primary bladder pain syndrome, formally termed interstitial cystitis, and chronic primary pelvic pain syndrome.
Chronic Primary Musculoskeletal Pain
The syndromes in this subcategory are labeled according to the site at which symptoms are evident (e.g. non- specific low back pain). These disorders were formally termed “non-specific” in formal nosologies, or attracted vague and imprecise labels in the community.
Conclusion
An understanding of the new and emerging nosology of pain may prove essential for insurance medicine professionals as the terms are adopted in the near future. The understanding will assist in assessing risk and adjudicating claims, as well as providing insight into current biological constructs underpinning the biopsychosocial facets of pain syndromes.
Part II of this article, which will be presented in the next edition of ReFlections, will focus on chronic secondary pain syndromes.