A basic principle in insurance is the concept of insurable interest. In life insurance, it means a policyholder must establish that he or she has an authentic financial interest in the person insured.
Pediatrics is the branch of medicine that oversees the health of a human being in his/her first years of life. Its scope includes newborn until adolescence.
Insurance products for children can include life, health, critical illness and personal accident covers. Disability products are not usual.
Living benefits policies for health and critical illness protect parents and children from the financial toll of a life-threatening illness. Health insurance plans can be diverse: some are built on a major expenses health insurance base; others cover hospitalization and/or surgeries on an indemnity base; and still others cover preventive medicine services.
Critical illness policies are also offered specifically for children. The list of insurable conditions for these policies should be clearly different than the product offered traditionally for adults. A typical juvenile CI policy can cover 30 or more conditions, with those most commonly included being cancer, type 1 diabetes mellitus, cystic fibrosis, hemophilia, Kawasaki disease, rheumatic fever with heart valve complications, encephalitis, major head trauma, major burns, and major organ transplants. Some female-specific CI products offer cover for pregnancy-related complications and certain congenital conditions, and would serve to provide some cover to the newborn child.
General personal accident insurance cover pays medical expenses due to an accident or pays a benefit for funeral expenses. These policies usually have low face amounts, and are acquired by individuals in a enrolled group such as a school or club.
In the case of life insurance for children, policies generally have small face amounts and the plans are structured as endowment or whole life. In certain markets, insurance can be purchased on the life of a child, but if the child dies before reaching age 14, no benefit will be paid and premiums will be returned. As an initial step in underwriting a child’s application an Agent’s Report should be obtained, showing how the sum insured was determined. Applications for large face amounts need to be evaluated carefully. The underwriting process information on the total amount of existing life cover on the child should also be taken into consideration, to avoid over-insurance. There are some general guidelines associated with pediatric underwriting
- Parent or parents should have insurance on their own lives of at least two times the amount of insurance of the child.
- The parents’ finances should be examined. Their income and net worth should not raise concerns of speculative intentions.
- All children in the same family should be insured equally. Whenever only one or some children in the same family are chosen for insurance, this should raise a red flag, as it could suggest possible anti-selection.
- The sum assured applied for must make sense in terms of policy type, term and reason for cover.
Pediatric Morbidity and Mortality
A child's growth and development can be divided into four stages:
- Infancy (0 - 2 years)
- Preschool years (3 - 5 years)
- Middle childhood years (6 - 12 years)
- Adolescence (13 - 19 years)
Each of these stages has its particular characteristics. Morbidity and mortality for each stage are different as well.
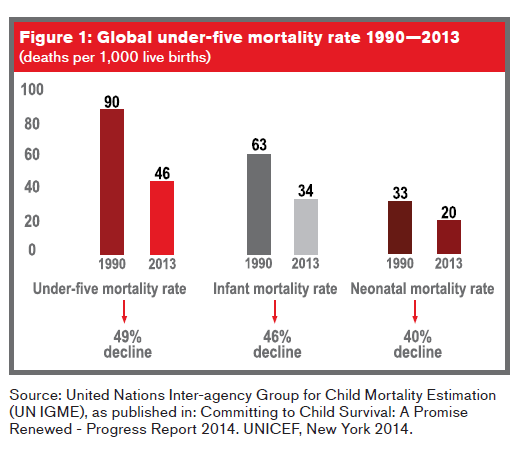
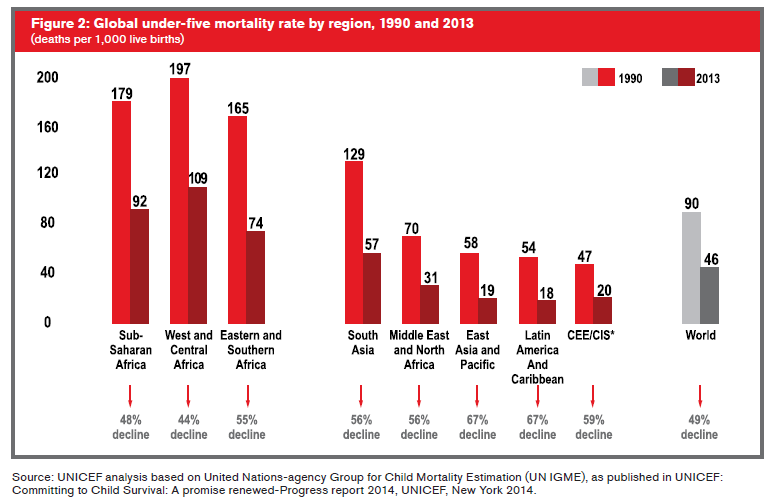
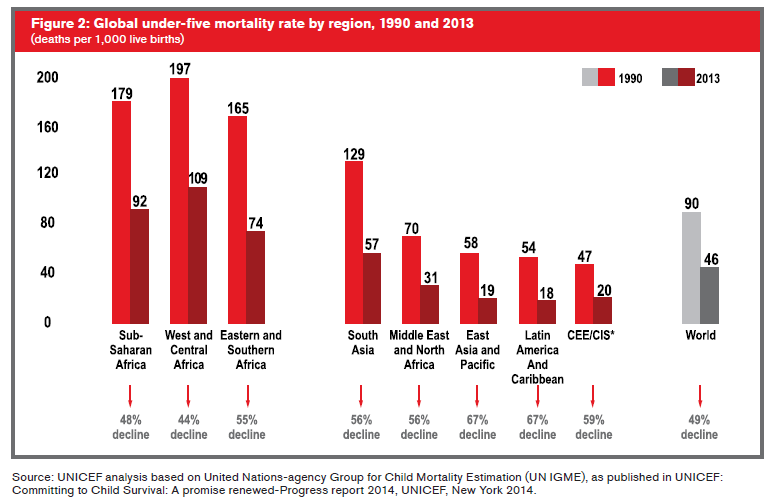
Substantial global progress has been made in reducing child deaths since 1990. According to the Levels & Trends in Child Mortality Report 2014, the global mortality rate for children under five years of age (infancy and preschool stages) has dropped 49% – from 90 deaths per 1,000 live births in 1990 to 46 per 1,000 in 2013. In addition, the global neonatal mortality rate (deaths occurring within 28 days of birth) declined by 40%, from 33 deaths per 1,000 live births in 1990 to 20 in 20131
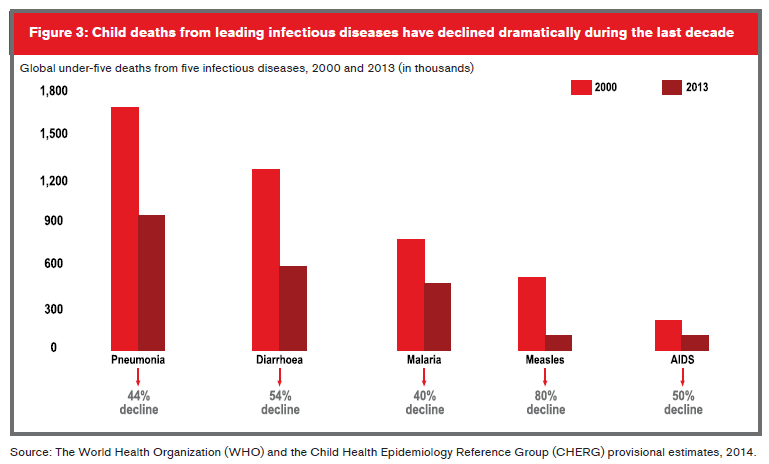
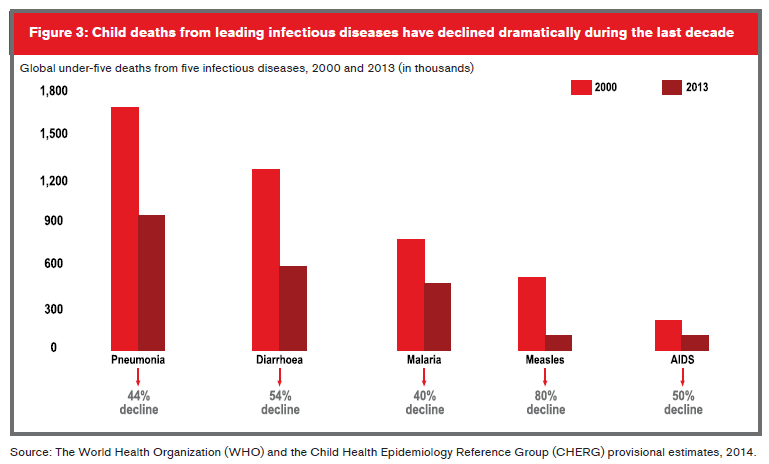
For children under the age of 5, the leading causes of death include: pre-term birth complications (17%); pneumonia (15%); intrapartum-related complications (complications during labor and delivery) (11%); diarrhea (9%) and malaria (7%). In addition, nearly half of under-five deaths globally are attributable to undernutrition2.
Prematurity
Prematurity used to be an important cause of neonatal mortality, but technological advances and improvements in medical knowledge in the field of neonatology have increased survival rates for premature babies. Still, the probability of death during the first week of life for babies born prematurely can be six times higher than for babies born after 37 weeks of gestation, and the probability for all premature infants to die before the age of one is three times higher3.
Expenses related to the care of premature babies have also increased. The average hospital stay for premature babies, often in intensive care, is three months. Expenses are not limited to this stage: some health problems can continue for many years. Several studies done in the U.K. show that expenses from hospital admissions accumulated during the first 10 years of life of children born prematurely are twice those of children born at term4.
In 2013, almost one million newborns (36%), whether full-term or premature, died the day they were born, and an additional one million (37%) died within six days of birth. Some 0.8 million neonatal deaths (27%) occurred between day 7 and day 27 of life1.
At least 90% of babies born after 28 weeks of gestation survive.
Prematurity can have long-term effects, including medical, developmental and/or mental problems or issues. These can continue until later childhood and can sometimes last into adulthood. Common long-term complications include:
- Bronchopulmonary dysplasia (BPD) (chronic lung disease). Premature babies might need oxygen for some months. Some improve slowly, while others can develop lung damage and pulmonary hypertension. These babies are also at major risk to develop respiratory infections such as pneumonia and bronchiolitis.
- Impaired growth and development.
- Mental or physical developmental delays or disabilities
- (intellectual disability, learning disabilities, cerebral palsy).
- Retinopathy, blindness.
- Loss of hearing.
In the long term, children born prematurely also have a higher risk of developing cardiovascular diseases, hypertension and diabetes as adults, and could also have a higher risk of developing cancer5 6 7.
Congenital Conditions and Abnormalities
Other important causes of morbidity and mortality in the first years of life are congenital conditions – defects that develop during pregnancy and are present at birth. They can be visible or microscopic, evident or occult, and can present sporadically or in several family members. In addition, they are not necessarily inherited.
Congenital abnormalities, such as malformations and genetic diseases, may cause chronic disabilities and can have a substantial impact on the affected, their families, health systems and society.
The list of these conditions and abnormalities is very long, and includes:
- Heart malformations
- Central nervous system malformations
- Inborn errors of metabolism
- Down syndrome
- Marfan syndrome
Causes of these conditions can vary. For example:
- Chromosomal abnormalities: Down, Turner, Klinefelter
syndromes - Genetic abnormalities: hemophilia, thalassemia, cystic fibrosis, Huntington’s disease, Marfan syndrome
- Environmental: a virus, or alcohol/drug use during gestation
Most congenital defects, unfortunately, do not have a recognizable cause. Among the most common congenital abnormalities are:
- Patent Ductus Arteriosus (PDA): This is one of the most frequent congenital heart malformations in children8. Diagnosis generally occurs at the pediatric stage, although approximately 2% of cases are discovered in adulthood. The condition leads to increased pulmonary blood flow and pulmonary arterial hypertension, manifesting clinically as cardiac failure, but it can also be asymptomatic. Treatment consists of the surgical or medical closure of the arterial duct. This defect was the first to be resolved surgically, and in recent decades its treatment has dramatically evolved.
PDA in premature and low-birth-weight children is associated with significant comorbidity and mortality due to hemodynamic instability. Asymptomatic patients with a small duct present a normal life expectancy, but they do have a life-long risk of endocarditis. Those with a moderate to large duct with important hemodynamic consequences can develop irreversible changes in the vasculature of the lungs and pulmonary hypertension.
Occasionally treatment does not take place in the pediatricage, which leads to the persistence of the patent arterial ductus into adulthood, which depending on the size of the short-cut, favors an increase in lung blood flow and the risk of vascular obstructive pulmonary disease (Eisenmenger syndrome). Mortality in adults, without treatment, is reported at 1.8% per year.
- Atrial and Ventricular Septal Defects (ASD/VSD):
These are also common congenital heart defects. VSD is the most common congenital heart defect, present in 14% to 17% of all babies born each year. ASD represents 6% to 10% of congenital heart defects, and is the most frequent cause (40%) of noncyanotic congenital heart disease in adults.
Children with this defect can be completely asymptomatic, and small septal defects usually close spontaneously and do not require treatment. Those affected should still be followed up with to ensure the defect has completely closed and that there are no complications, for they may become symptomatic in adult life. Complications from ASD are arrhythmias, especially atrial fibrillation, heart failure, endocarditis, pulmonary hypertension and strokes. Complications from VSD are aortic regurgitation, heart failure, endocarditis, and pulmonary hypertension.
- Central nervous system congenital abnormalities:
These constitute important causes of disability among children. They include neural tube defects such as anencephaly, encephalocele and spina bifida, which are the most frequent central nervous system malformations, with prevalence varying between 0.8 - 1 for every 1,000 babies born alive. Genetic and environmental causes include maternal folic acid deficiency, maternal exposure to rubella virus and to valproic acids, radiation, and folic acid antagonists such as trimethoprim, carbamazepine, phenytoin and phenobarbital. The rate of occurrence for neural tube defects is 1.5% - 5%, and for anencephaly alone can reach 10% 9, 10. The prognosis for brain malformation depends on the severity. For anencephaly, the prognosis is always fatal. Encephaloceles are classified depending on the region involved. Long-term evolution shows high mortality, and most of the survivors have severe disabilities.
Spina bifida (meningocele or myelomeningocele) has an incidence of 1/1000. This defect can be closed (15%) or open (85%). Hydrocephalus is the most important complication for lumbo-sacral myelomeningoceles and is present in 90% of cases, and Chiari II malformation is present in 70% of cases. Other associated abnormalities include hip dislocation, foot deformities, contractures or flaccid paralysis. A child’s ability to walk varies with the level of the spina bifida lesion. In any case, the child should receive physical therapy, and orthopedic surgery may be necessary to enable the child to stand upright and be ambulatory. Other concerns are elimination functions: there is also a high risk for urinary tract infections and bowel dysfunction as poor peristalsis predisposes to constipation. Intellectual capacity in children with neural tube defects is in a wide range; however, most are at low-normal to borderline levels.
With adolescence, scoliosis may become apparent and be associated with syringomyelia. Kidneys might be affected due to chronic recurrent infections and calculus, and lead to loss of renal function. Affected individuals may become obese and less ambulatory. The transition into independent adulthood is very difficult, and psychosocial problems are major.
When the spina bifida defect is closed health problems may be similar, but hydrocephalus is rare and intelligence is usually normal.
- Down Syndrome: This condition is due to chromosomal abnormalities, and its most constant characteristic is intellectual disability: IQs vary between 20 and 80. The great majority (95%) of Down syndrome infants have a 21 trisomy (extra copy of chromosome 21). In 4% of sporadic cases and 1/3 of familial cases the affected child has 46 chromosomes, which includes an abnormal chromosome 21. Mosaicism of the 46/47 type can also occur, and may have milder symptoms.
About one-third of children with Down syndrome have congenital heart disease, and most have a septal defect. Leukemia is 20 times more common than in unaffected children. Other complications these children can present and which becomes more common as they grow older include infectious diseases due to abnormalities in their immune system, dementia, seizures, Alzheimer’s disease, sleep apnea, obesity, hearing and vision problems, and thyroid dysfunction.
Life expectancy for these individuals has improved dramatically; people with this condition can now live to age 60 or older. Generally, children with Down syndrome reach key developmental milestones later than other children.However, with appropriate support and treatment, many with Down syndrome lead happy, productive lives.
- Marfan syndrome: This is a connective tissue disorder caused by a genetic defect. In the majority of cases it is inherited, but up to 30% of the patients have no family history. In this disease there is a progressive involvement of organs and systems: skeletal, cardiovascular, ocular, skin, lungs. There are three forms of presentation:
- Neonatal Marfan: Very few cases have been reported. Prenatal ultrasounds will show cardiomegaly with severe tricuspid regurgitation, and at birth there are skeletal and skin abnormalities (long limbs with delicate fingers, the appearance an elderly individual, hypotonia) and cardiovascular lesions (mitral and tricuspid severe regurgitation, cardiomegaly, aortic and pulmonary dilation, arrhythmias, mitral prolapse, ascending and descending aortic aneurysms). Death occurs in hours or days from heart failure.
- Infantile Marfan: Usually seen in children before the age of 16. The non-cardiac manifestations are arachnodactyly, facial and palate abnormalities,scoliosis, and chest deformities. Cardiovascular lesions are present in 55% of the cases, and most are asymptomatic. Aortic dilation is found in 42% ofthe affected children, and most of the patients have cardiovascular compromise when reaching skeletal maturity. The most common cardiovascular lesions are mitral prolapse, aortic root dilation and mitralregurgitation. In this type of Marfan, average age of death is 16.3 months, and 74% have heart failure. During the early ages, morbidity and mortality are more related to mitral valve disease and in later childhood/adolescence, to aortic valve compromise
- Classic Marfan: This is the most frequent and known presentation and can be found in children, adolescents and adults. Cardiovascular diseases are the most important cause of mortality and the most common of them is aortic dilation. Its incidence depends on age: 40% - 80% in children and 80% - 100% in adults. It has a negative prognosis due to its progressive nature,leading to valvular incompetence, dissection and rupture. In 70% of the cases one sees progressive eye problems: crystalline subluxation, glaucoma, cataracts, and retinal detachment.
- Inborn Errors of Metabolism: These genetic disorders were first described at the beginning of the last century and were considered rare. Since then, the number of known inborn errors of metabolism has increased and now are known as important causes of pediatric-age disease. In some cases effective treatment is available. In others, however, even though there is no known treatment, informed decisions about future offspring can be made. Clinical manifestations can vary. Common situations are acute metabolic disease in the newborn (which can be confused with sepsis), intellectual disability, vomiting and encephalopathy in an infant or older child, hypoglycemia, hyperammonemia or acidosis at any age.
Accidents
Unintentional injuries are the leading cause of death among children and adolescents, accounting for nearly a third of all deaths among children between the ages of one and 14, and more than four in ten of all deaths among teens ages 15 to 19. Most injuries and deaths of children due to accidents happen in the home or on the streets, in schools, or at recreation centers.
Accidents with young children usually occur at home, and are the result of falls, mouth burns (from food heated in microwave ovens), electrical burns (on hands), choking, asphyxiation or drowning, and amputation of a finger. As children grow older and are standing up and walking, the risk of a different type of injury increases. In addition to the previously mentioned causes, children can swallow foreign objects (coins, small toys), experience boiling water burns and esophageal burns due to the ingestion of caustic substances, suffer dog bites and traffic-related injuries, or while they are in a vehicle, experience head, chest and/or abdominal trauma.
At preschool age, a child’s range of activities increases and so does the accident risk. In this age range, accidents can result from the use of bicycles, skates and skateboards, causing fractures and serious head, chest and abdominal trauma.Going to school increases the possibility of sports injuries. During adolescence, there is an increase in injuries due to sports, moving vehicles (bicycles, motorcycles, cars) and guns.
Traffic-related injuries are highest for children from 5 to 19 years of age. In teenagers, lifestyle-related issues such as use of alcohol, drugs and participation in dangerous avocations should be considered. Severe head trauma is present in 80% of accidental deaths in children. Boys are more likely than girls to experienceinjuries and to die as a result of an injury. The difference exists regardless of the child’s age and across all OECD countries. It may relate to differences in behavior, or in the type of activities in which boys and girls engage11.
Cancer
From ages 5 to 14, a third leading cause of death is cancer. The most common types of cancer in children are different from those seen in adults. They are: leukemias, brain and other central nervous system tumors, neuroblastoma, Wilms’ tumor, lymphomas, rhabdomyosarcoma, retinoblastoma and bone cancers (i.e., osteosarcoma and Ewing’s sarcoma).
Lifestyle-related risk factors seem to play a major role in many types of cancer in adults and usually take many years to influence. In childhood cancers, however, lifestyle factors do not seem to play a role. There may be some environmental factors, such as radiation exposure, but in most cases external cause has not been demonstrated. Some children inherit mutations that increase their risk to develop cancer and the cause is not known.
Each year in the U.S. approximately 13,400 children between birth and 19 years of age are diagnosed with cancer. About one in 300 boys and one in 333 girls will develop cancer before reaching age 20. In 1998, cancer was the most common cause of death by disease for children and adolescents.
While the incidence of childhood cancer has changed only slightly, the overall survival rate for childhood cancer has increased drastically. Today, the overall five-year survival rate for childhood cancers is close to 80%. Because treatment cure rates have increased, the population of childhood cancer survivors has also increased. Currently there are estimated to be 270,000 such survivors in the U.S. This equates to one in 640 young adults between the ages of 20 to 39 being a survivor of childhood malignancy. Survival has its cost, however: two-thirds of those who survive will later face at least one chronic health condition (heart or lung damage, second cancer, infertility, cognitive impairment, growth deficits among others)12.
Underwriting
Underwriting a child’s risk may already be challenging even when the child is apparently healthy. A child has a longer life expectancy, is still undergoing changes due to ongoing growth and development, and is constantly experiencing the effect of environmental physical, biological and social influences.
In making an underwriting assessment of a child, an underwriter should consider the prenatal and neonatal history as well as whether the pregnancy and delivery were normal or if there were complications. It is important also to review parental lifestyle issues (e.g., whether use of tobacco, alcohol and/or drugs was present), as well as parental occupational hazards.
Infectious disease risk in children can be prevented through proper immunization. It is important to consider insurability of children whose parents have chosen not to vaccinate them. Red flags are expressed parental concerns about autism and the measles-mumps-rubella (MMR) vaccine, multiple sclerosis and the hepatitis B vaccine, and sudden infant death syndrome and the diphtheria-tetanus-pertussis vaccine, despite scientific evidence that does not support these associations. Some juvenile critical illness policies cover infectious diseases such as polio, and a valid question is whether a claim for childhood polio should proceed in cases where parents have chosen not to provide the vaccine.
Physical growth and development of psychomotor milestones should also be considered in the course of underwriting. Just as underwriting for the elderly should introduce cognitive testing, an age-appropriate approach should be taken when considering an insurance application for a child.