Key takeaways
- The breakthrough treatment employed base editing technology to correct a single mutation – a precision approach that minimizes side effects while addressing the fundamental genetic defect.
- This approach could dramatically reduce costs of gene-editing treatments and eventually extend to more common genetic disorders such as sickle cell disease, cystic fibrosis, Huntington's disease, and muscular dystrophy.
- With the implementation of this technology, morbidity and mortality risk from life-altering genetic conditions will improve significantly.
CPS1 deficiency is an ultra-rare disorder affecting less than one in one million newborns, with a grim prognosis – half of affected infants have a significantly increased risk of mortality within the first week of life. Survivors typically face severe neurological impairment and eventually require liver transplantation.
The groundbreaking case of a child who was recently cured of the life-altering symptoms related to this genetic condition represents a pivotal moment in genomic medicine with profound implications for rare genetic disease management. The successful development and implementation of a personalized base editing treatment for CPS1 deficiency highlights several key considerations, which this brief explores.
A remarkable success story
In this case, treatment resulted in remarkable clinical improvement: The infant's protein tolerance normalized, medication requirements decreased substantially, and the patient showed resilience against intercurrent illnesses that would typically trigger life-threatening hyperammonemia. Growth parameters improved from the 7th to the 40th percentile, and developmental milestones are being met without daily management using medications, supplements, or dietary modifications.
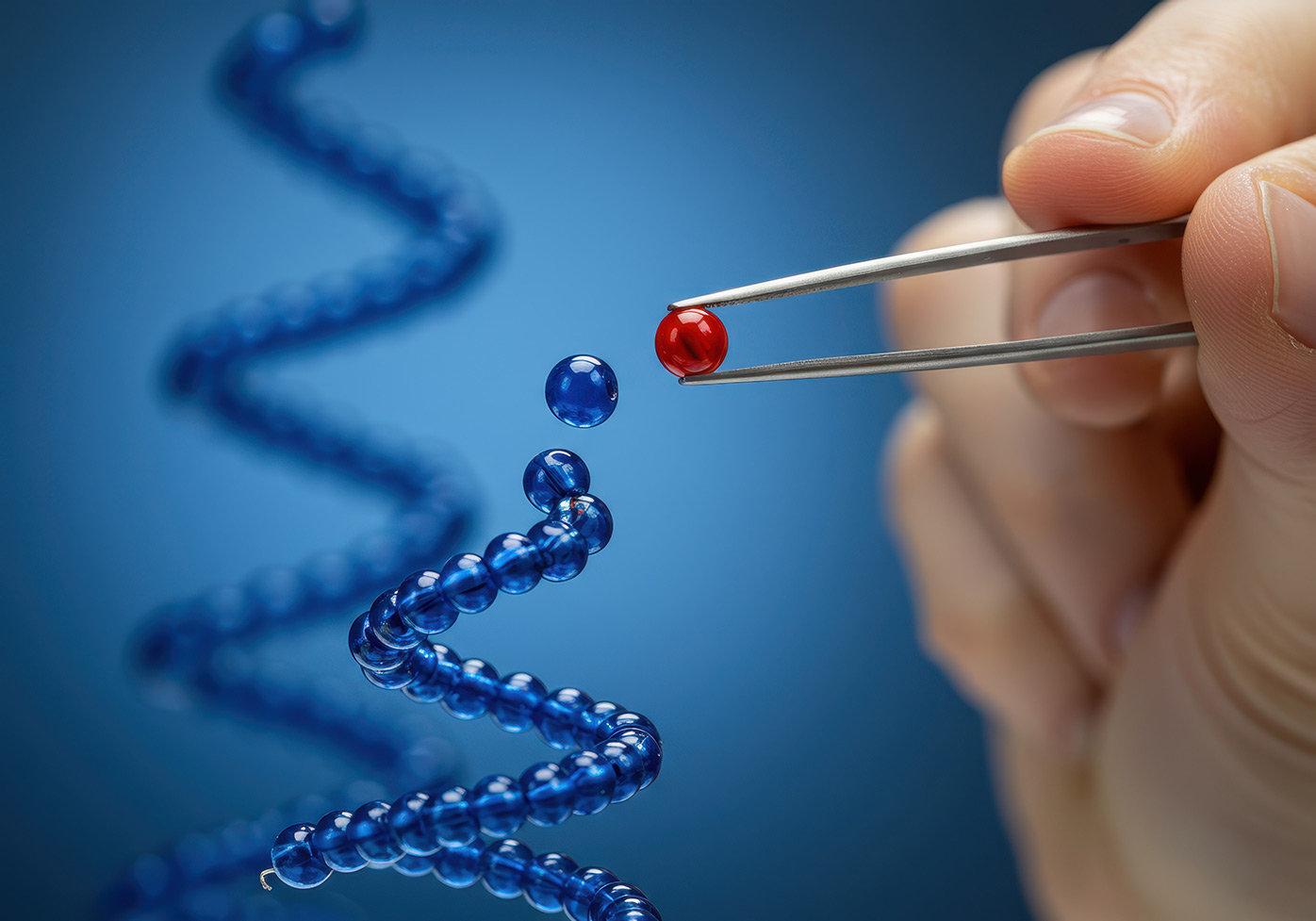
The treatment employed base editing technology to correct a single nucleotide mutation. The therapeutic payload was delivered via lipid nanoparticles and contained a modified CRISPR system functioning as a molecular "GPS" to precisely locate the mutation, along with instructions for cells to produce the editing enzyme. This precision approach minimizes off-target effects while addressing the fundamental genetic defect.
Interestingly, the therapeutic framework is potentially adaptable to thousands of other rare genetic disorders as long as the CRISPR "GPS coordinates" are modified to target different mutations; the delivery system and editing mechanisms could remain largely unchanged. Dr. Peter Marks, former FDA official, notes this approach could reduce costs "by an order of magnitude at least" and eventually extend to more common genetic disorders such as sickle cell disease, cystic fibrosis, Huntington's disease, and muscular dystrophy.
Development timelines for this approach were dramatically compressed – work that traditionally takes several years was accomplished in months through extraordinary collaboration.
Scaling this model will require robust systems for rapid gene sequencing and mutation characterization, streamlined regulatory pathways for individualized treatments, expanded manufacturing capabilities for customized genetic medicine, and frameworks for equitable access to highly personalized therapies.
Future considerations
The case raises important ethical questions about resource allocation, equity of access, and prioritization in healthcare. While this innovative approach offers hope to families affected by rare disorders, ensuring fair distribution of such resource-intensive treatments will be challenging.
In the US alone, 30 million people are affected by approximately 7,000 rare genetic diseases. This case establishes a precedent for developing personalized genetic treatments without the extensive development timelines that have historically discouraged investment in ultra-rare conditions. With the implementation of this technology, morbidity and mortality risk from life-altering genetic conditions will improve significantly.
The collaborative model demonstrated here – involving academic researchers, multiple companies, and regulatory authorities – provides a template for future efforts. The success underscores the value of sustained investment in basic science research and translational genomic medicine.
RGA has long served as a leading industry voice on the advances in genomic medicine and their implications for life and health insurers. We invite you to engage with our experts to prepare for this new era of medical innovation. Interested? Contact RGA.