According to New York State Department of Health, around 60% of those in New York who died from COVID-19 were male.
The European Centre for Disease Prevention and Control (ECDC) reported that the male-to-female ratio for COVID-19 deaths across the EU was 2.1. The U.K.’s Office for National Statistics (ONS) reported that rate of death due to COVID-19 for males was double that of the rate for females. For reasons that remain unclear, the novel coronavirus appears to present a significantly higher mortality risk to men than women.
In this paper we investigate how COVID-19 mortality risk differs between men and women across different age groups and different countries. A better understanding of the relationship between age, sex, and COVID-19 mortality, and how this differs by country, will help us to:
- Stratify COVID-19 mortality risk within a population
- Understand why there are differences in COVID-19 mortality rates among countries
- Understand how COVID-19 mortality risk for insured populations may differ from general population risk, due to differences in age and sex profiles
We extract publicly available age- and gender-stratified COVID-19 death data for Australia, Belgium, Germany, Italy, the Netherlands, South Korea, Spain, the U.K., and the U.S. Using these data, we explore COVID-19 mortality rates for males and females across different age segments and compare them with all-cause mortality rates taken from the Human Mortality Database.
We show that COVID-19 mortality rates differ by age and sex in the nine countries studied. The male-to-female differences in COVID-19 mortality rates were observed to be greater and have a bigger variation than the differences in all-cause mortality rates, although part of this may be due to low data volumes at some ages in some countries. COVID-19 mortality rates exponentially increase by age for both males and females. The male COVID-19 mortality rate is generally higher than the COVID-19 female mortality rate across all ages in the countries investigated. The age shape is broadly similar by sex within a country, although there were some notable differences between countries.
Finding, extracting, and analyzing COVID-19 deaths data
Publicly available data sources
The totals for COVID-19 reported deaths by sex and age were extracted from the following sources:
It is important to note that what counts as a COVID-19 death differs by country. Most countries currently include only deaths in hospitals, although some countries may include deaths outside of the hospital setting and the definition may change over time. See the Appendix for a fuller discussion on the data limitations.
The date shown in the table is the date of the source report used for each country. Data were compiled on July 3, 2020. Age segments younger than 40 years were excluded due to lack of COVID-19 death data. Death data for Germany, the U.K., and the U.S. were smoothed into age segments of 10 years (assuming the counts followed a Weibull distribution by age).
The age- and sex-stratified population data for year 2020 were extracted from the Department of Economic and Social Affairs, United Nations. This was used to calculate the mortality rate of COVID-19 for each segment.
The male-to-female ratio of the COVID-19 mortality rate was compared to the corresponding male-to-female ratio of the population all-cause mortality rate. The age- and sex-stratified all-cause death and population data were extracted from the Human Mortality Database. This was used to calculate the all-cause mortality rate at the population level for each segment. The confidence interval was calculated using the delta method.
Calculating the mortality rate
The mortality rate (per 1,000 population) for each age segment, X, was calculated separately for males and females as follows:
Calculating the gender mortality ratio
The gender mortality ratio (GMR) for each age segment, X, was calculated as follows:
COVID-19 mortality rates by age and gender from around the world
COVID-19 mortality rate
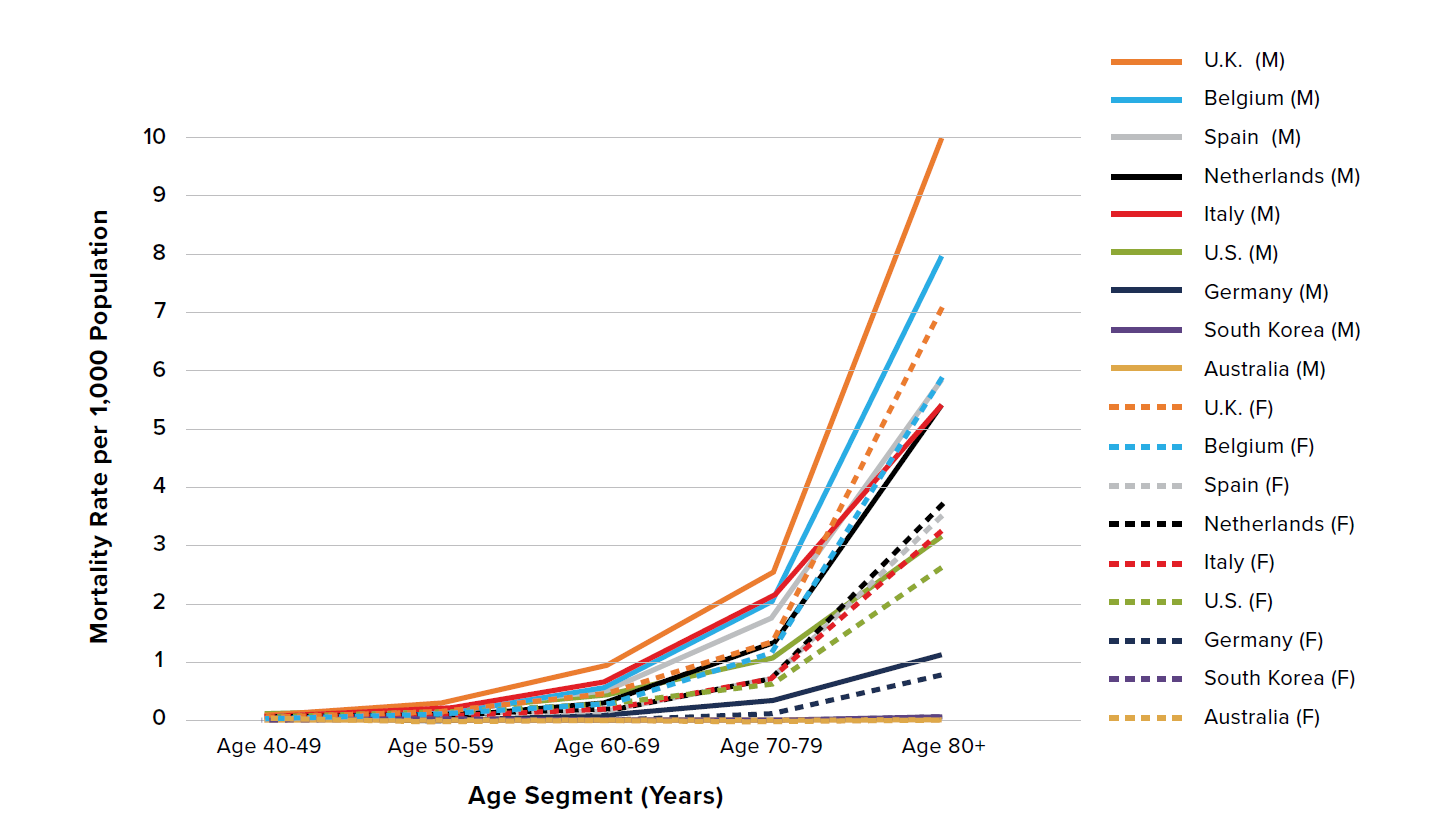
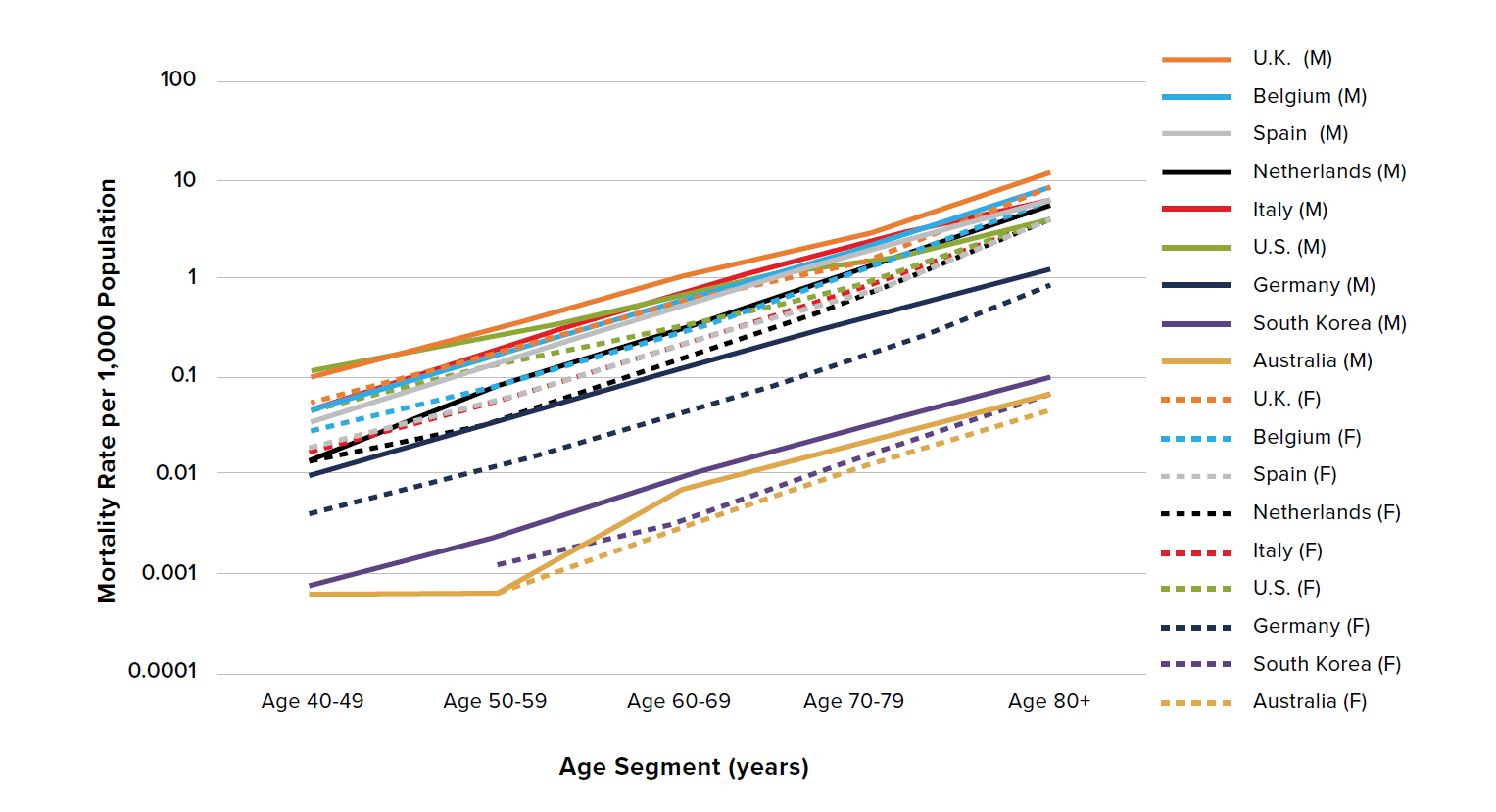
Figure 1 shows COVID-19 mortality rates per 1,000 population by age and sex in adults aged 40 years and older for the U.K., Belgium, Spain, the Netherlands, Italy, the U.S., Germany, South Korea, and Australia.
Figure 1:
COVID-19 mortality rates per 1,000 population by age and gender in adults aged 40 years and older
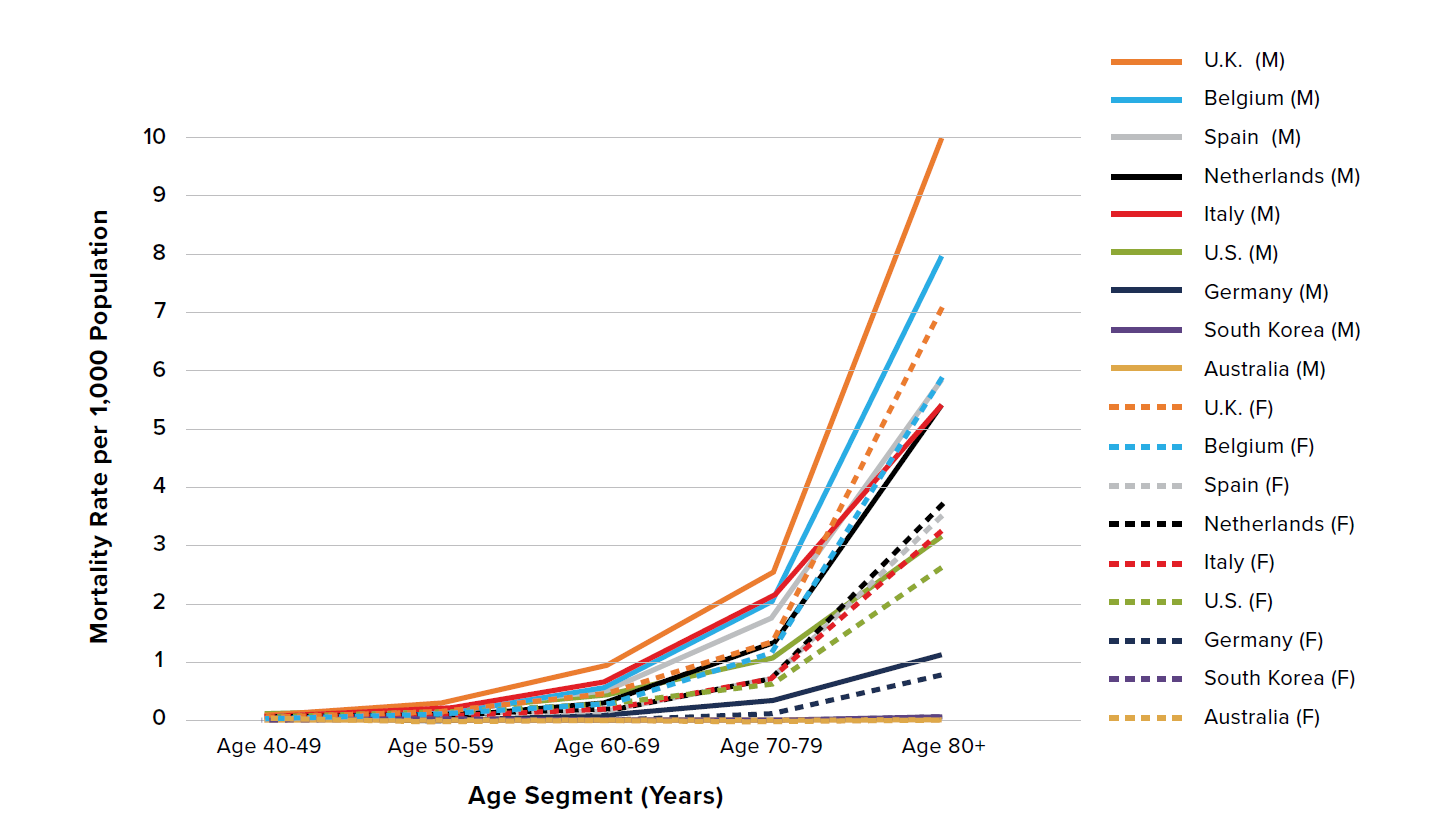
Figure 2 presents the data in Figure 1 on the log10 scale. Note the broadly similar shape of the lines representing the mortality rates for males and females within each country, demonstrating that mortality risk exponentially increases by age similarly for both men and women. However, there are differences between countries – for example, the difference in slope between males (solid lines) in Italy and the Netherlands indicates a variation in the mortality rates for those countries.
There are two observably distinct groupings: South Korea and Australia comprise a subgroup that exhibits lower overall mortality rate, while the U.K., Belgium, Spain, the Netherlands, Italy, the U.S., and Germany exhibit higher overall mortality rates.
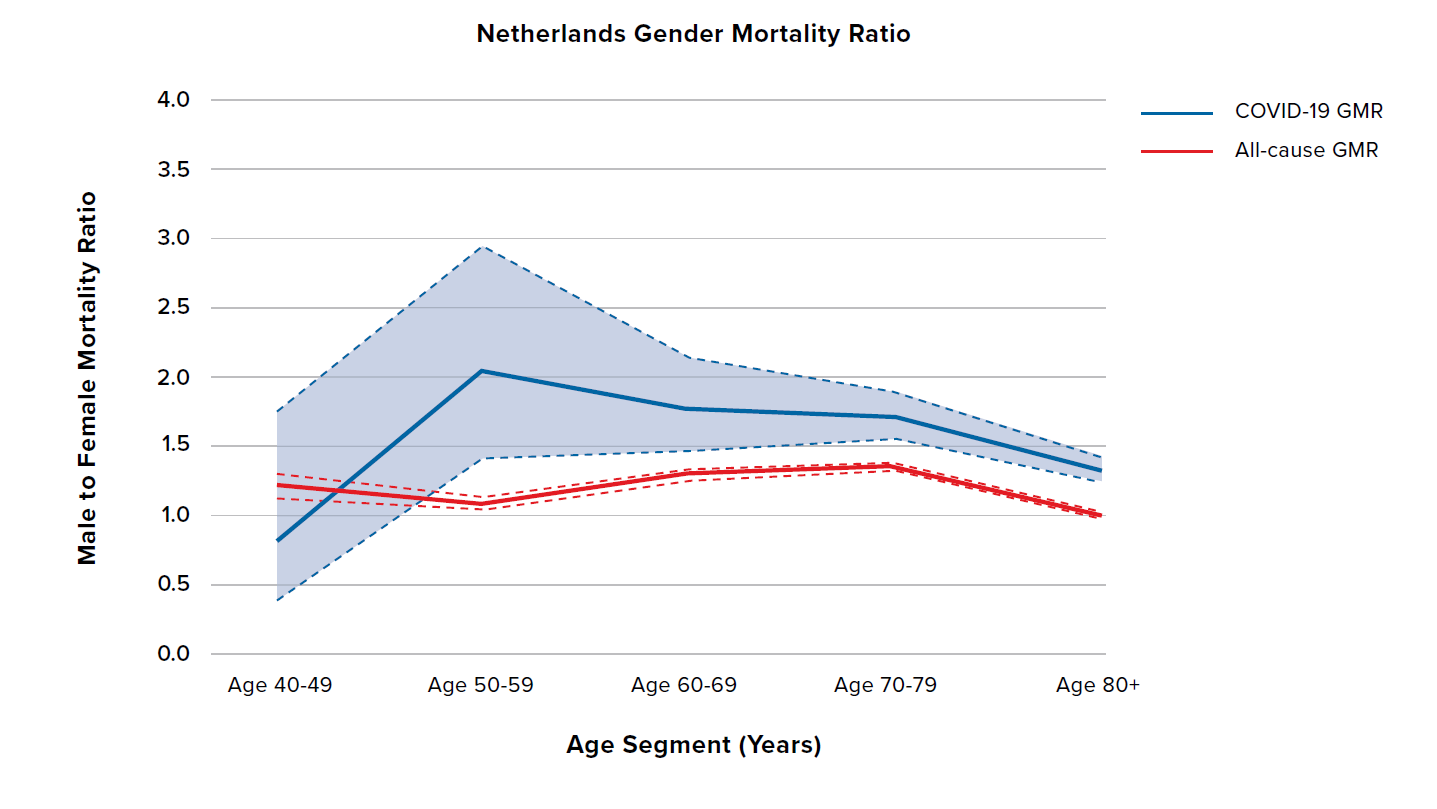
Male mortality rates are consistently higher than female mortality rates across all age groups aged 50 and older, regardless of the overall level of mortality. The same holds true for ages 40 to 49 with the exception of the Netherlands, which may be due to low levels of data.
COVID-19 gender mortality ratios
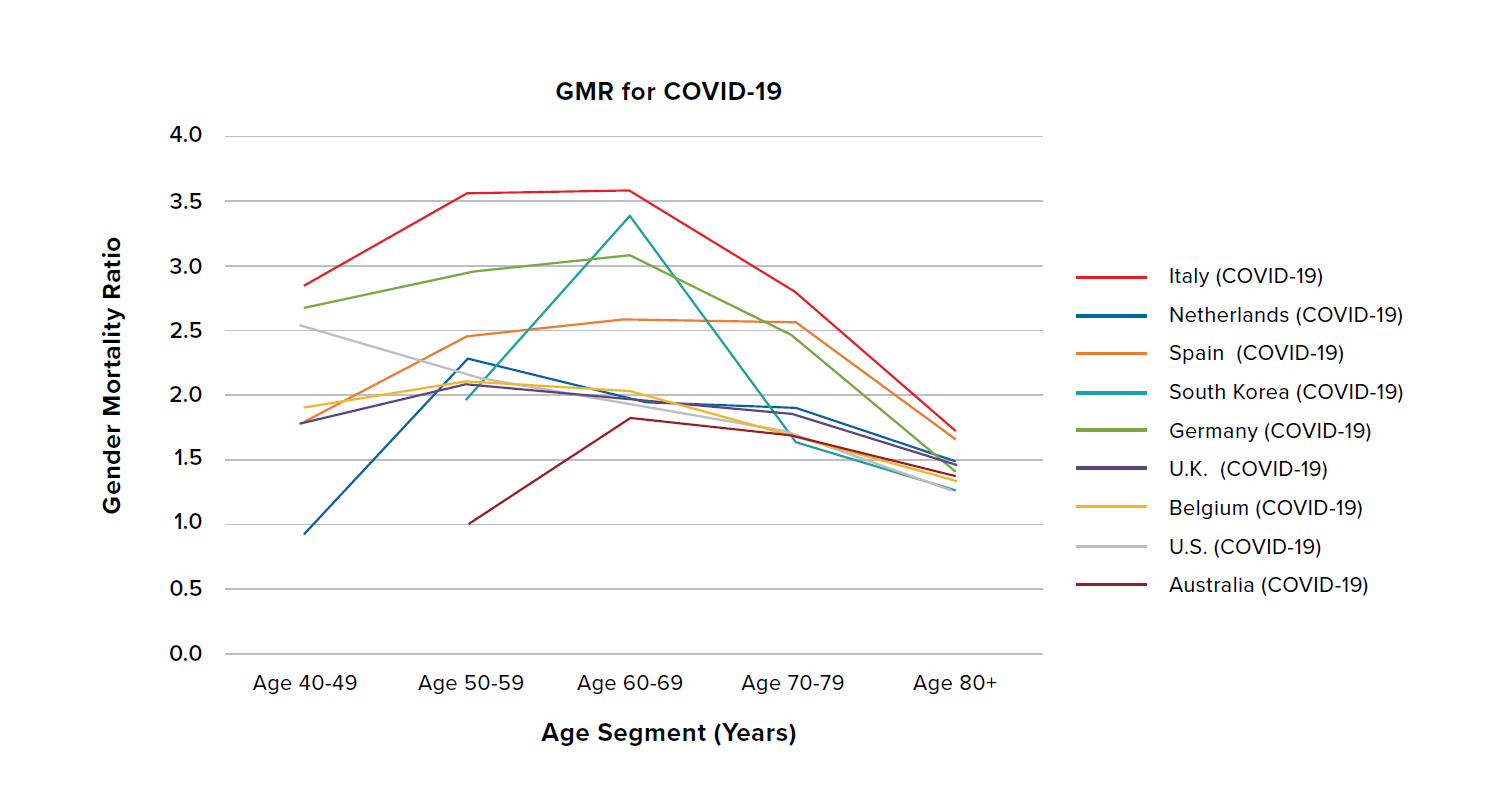
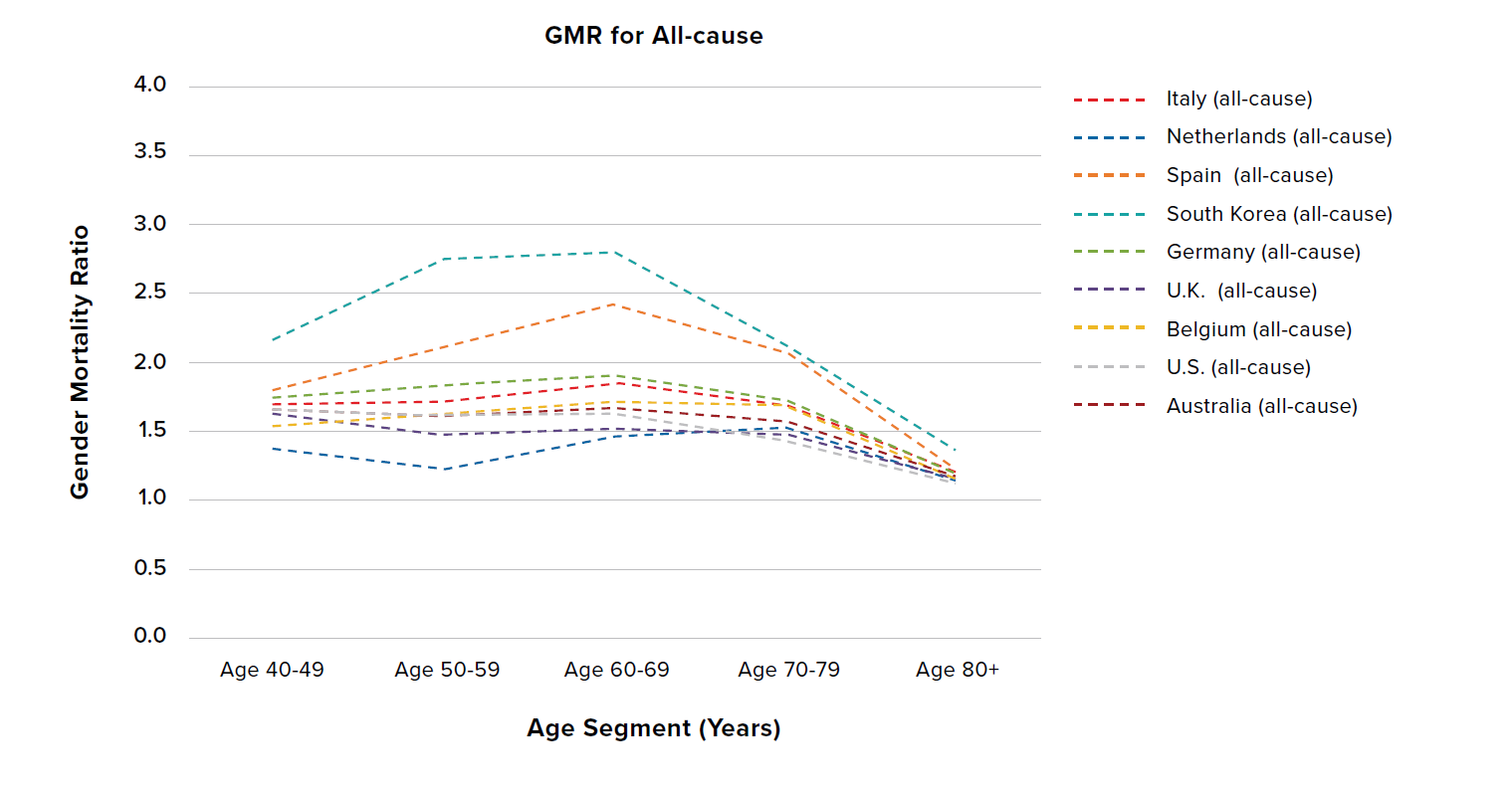
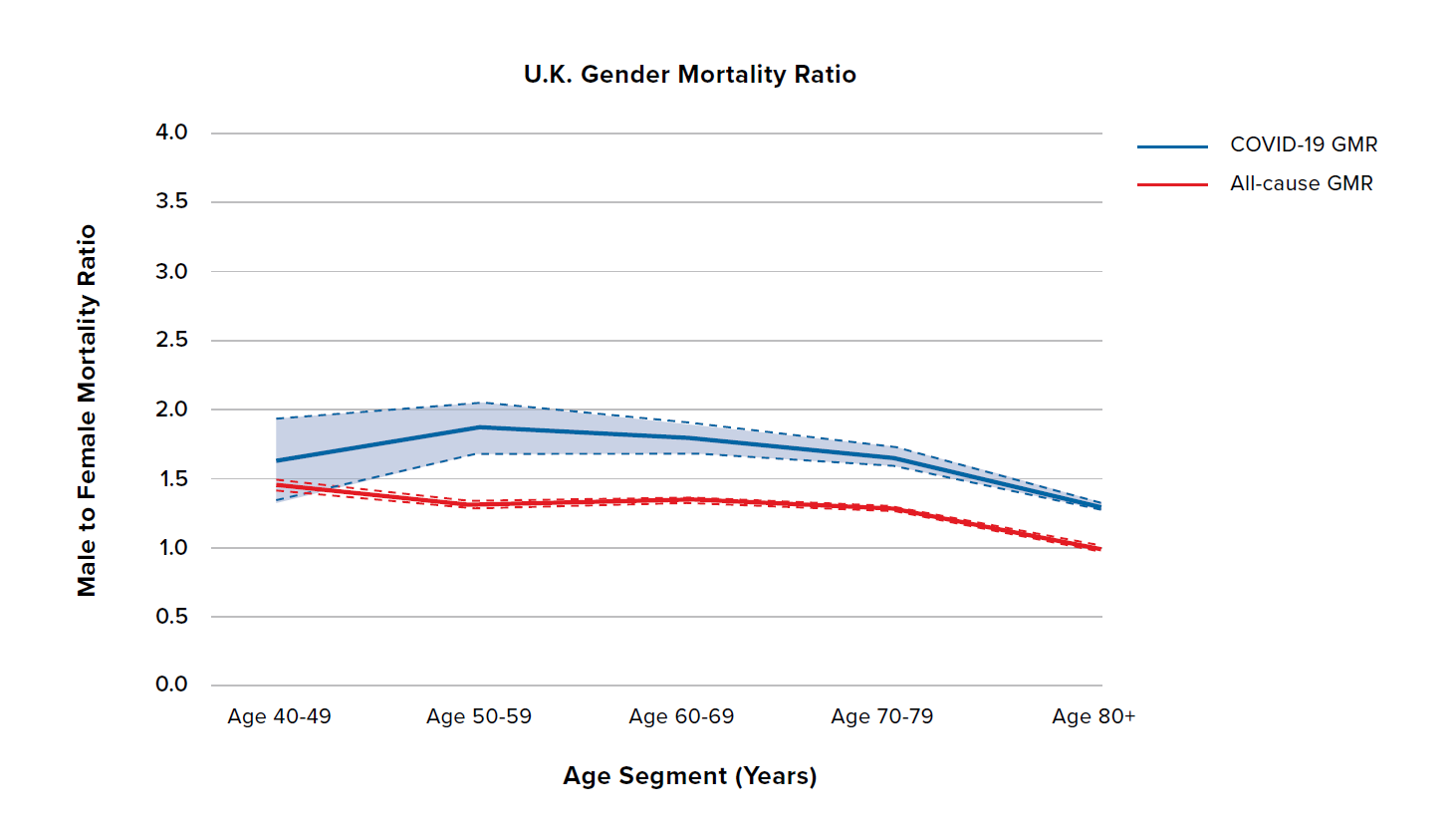
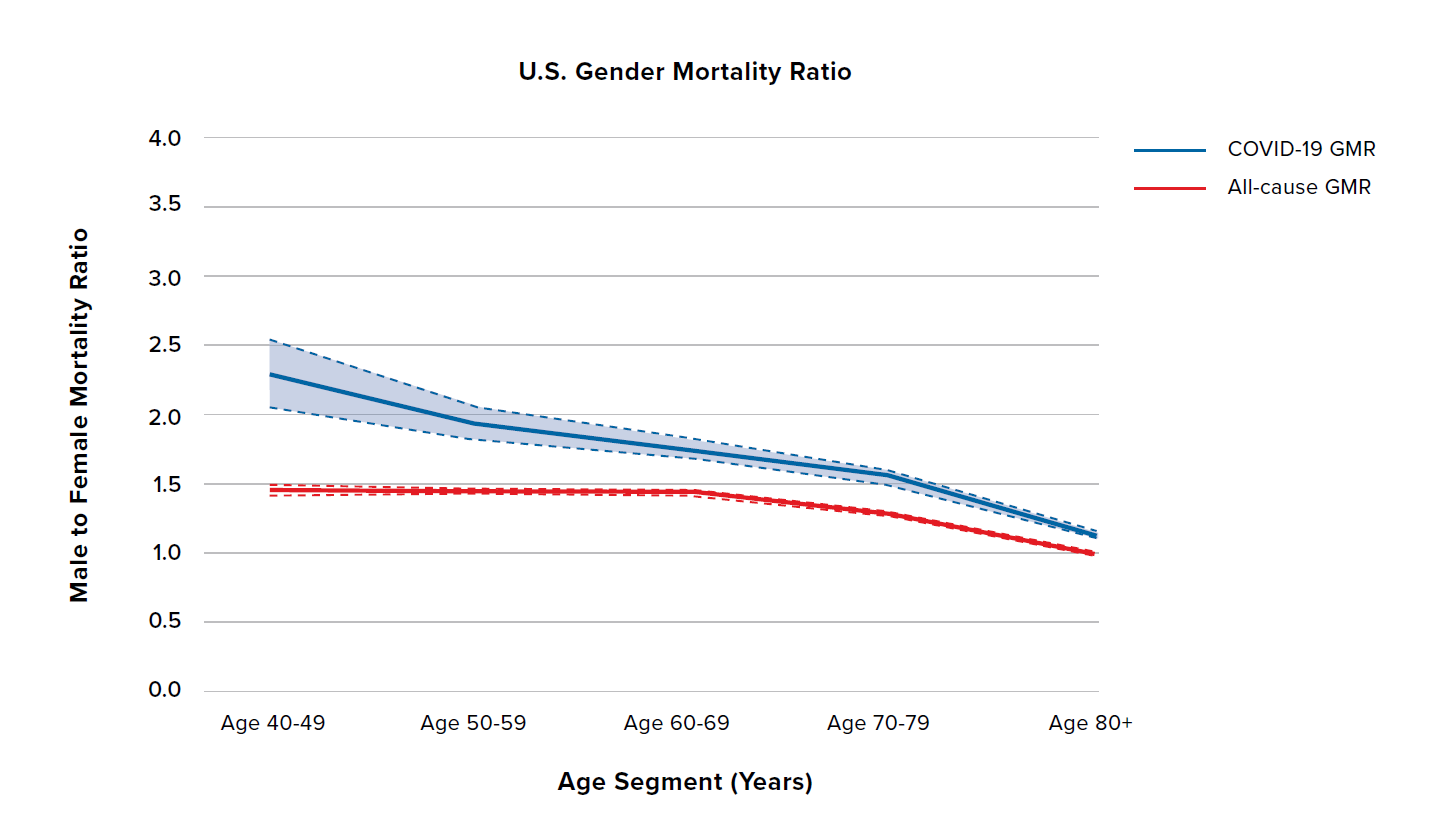
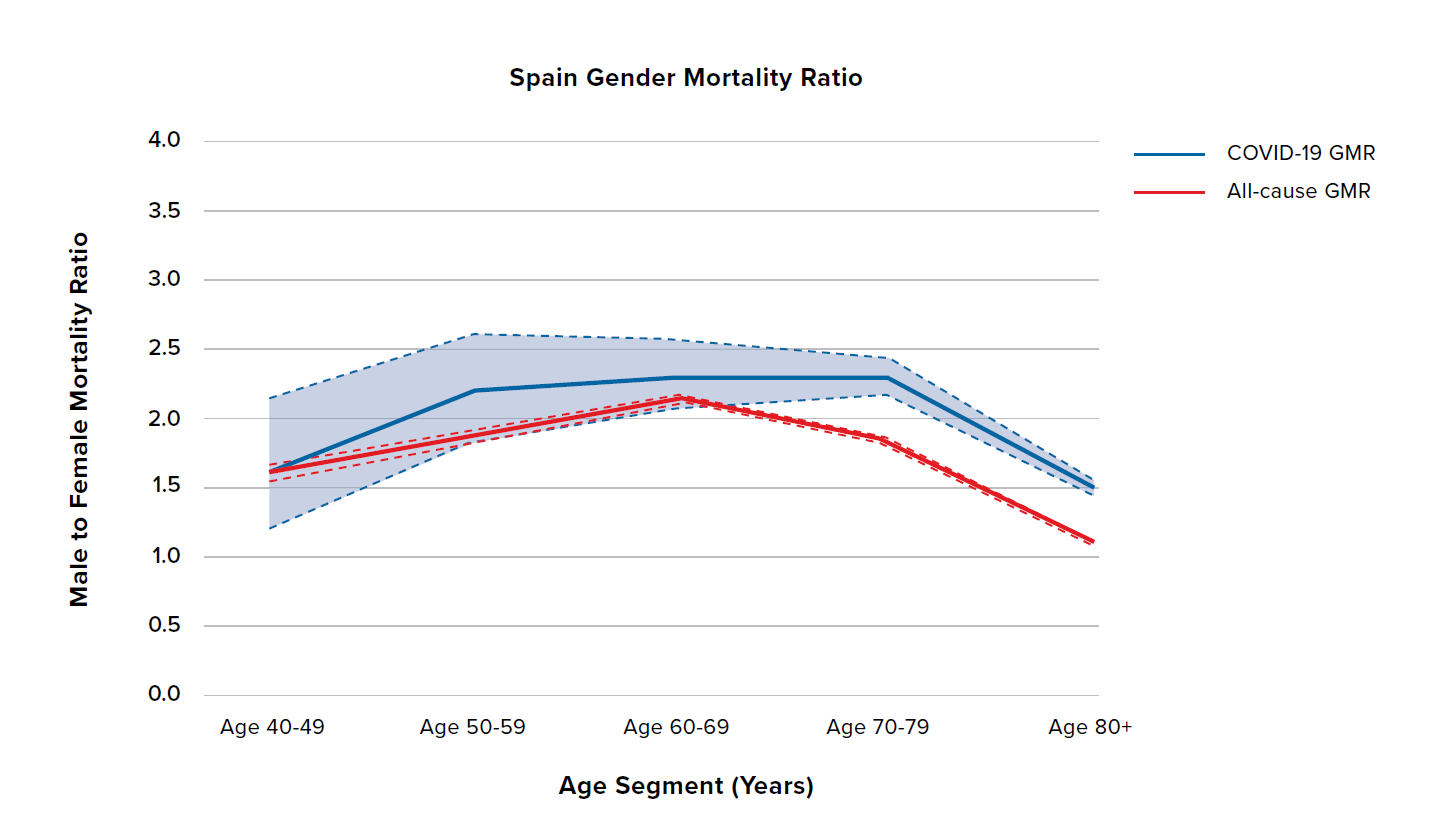
The left side of Figure 3 shows the age-stratified gender mortality ratio (GMR) of COVID-19 mortality rates (solid lines), while the right side shows the all-cause mortality GMR (dashed lines). To better view and compare data from specific countries, we have split the data into three country groupings in Figures 4, 5, and 6. Four interesting features can be seen in Figure 3:
- The COVID-19 GMR is generally higher than the all-cause GMR, suggesting that there is a bigger sex differential in COVID-19 than in all-cause mortality.
- This sex differential differs by country – see how the magnitude of COVID-19 GMR compared to all-cause GMR varies significantly by country.
- The all-cause GMR converges at ages 80+ to a ratio between 1.1 and 1.3, demonstrating a diminishing difference between male and female mortality rates at old ages. While the COVID-19 GMR exhibits convergence at ages 80+, the ratio is higher at between 1.2 and 1.9.
- South Korea and Spain have notably higher all-cause GMRs than the other countries.
Figure 3:
COVID-19 (solid lines) and all-cause (dashed lines) GMRs by age in adults aged 40 years and older for nine countries
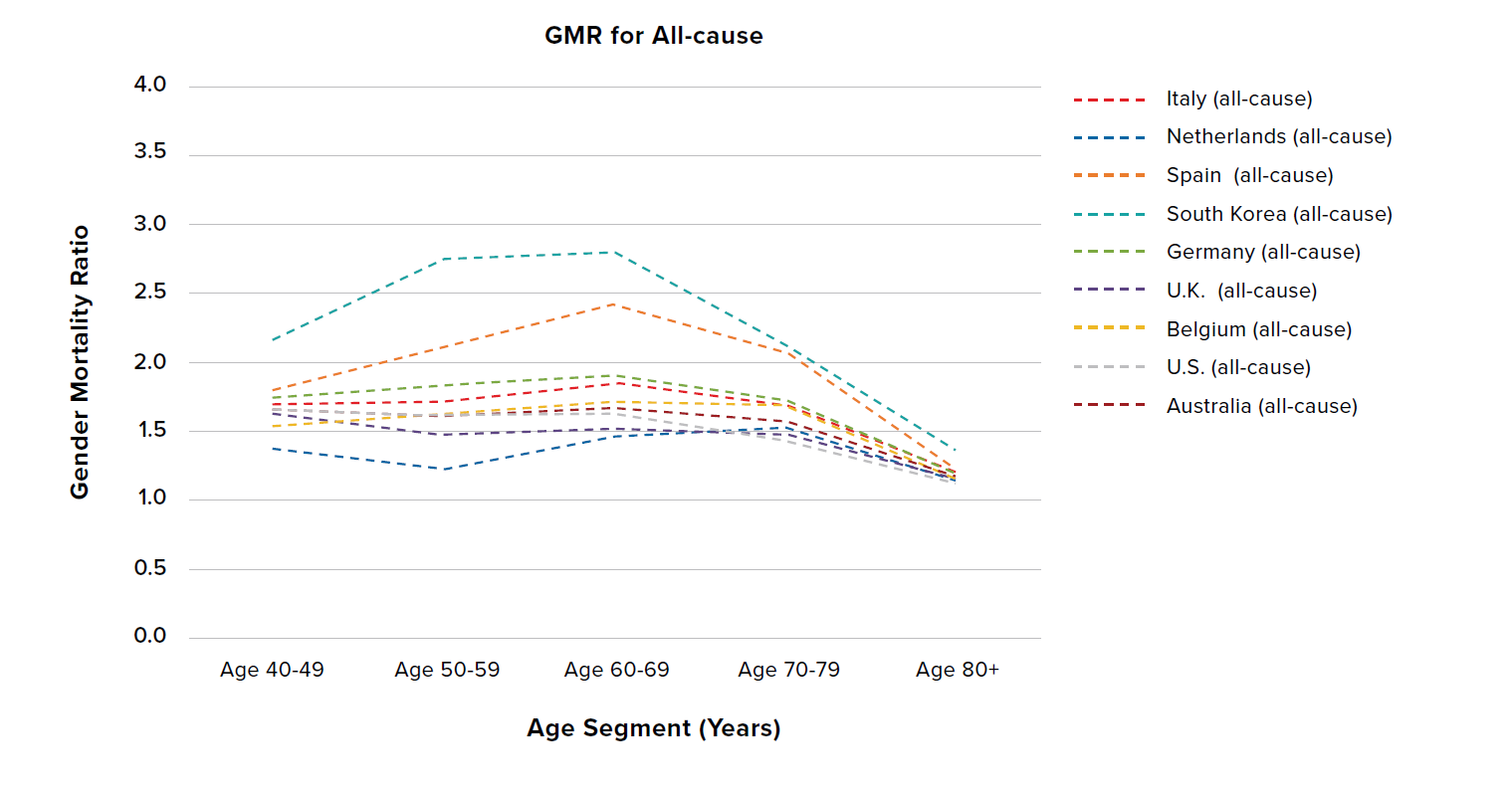
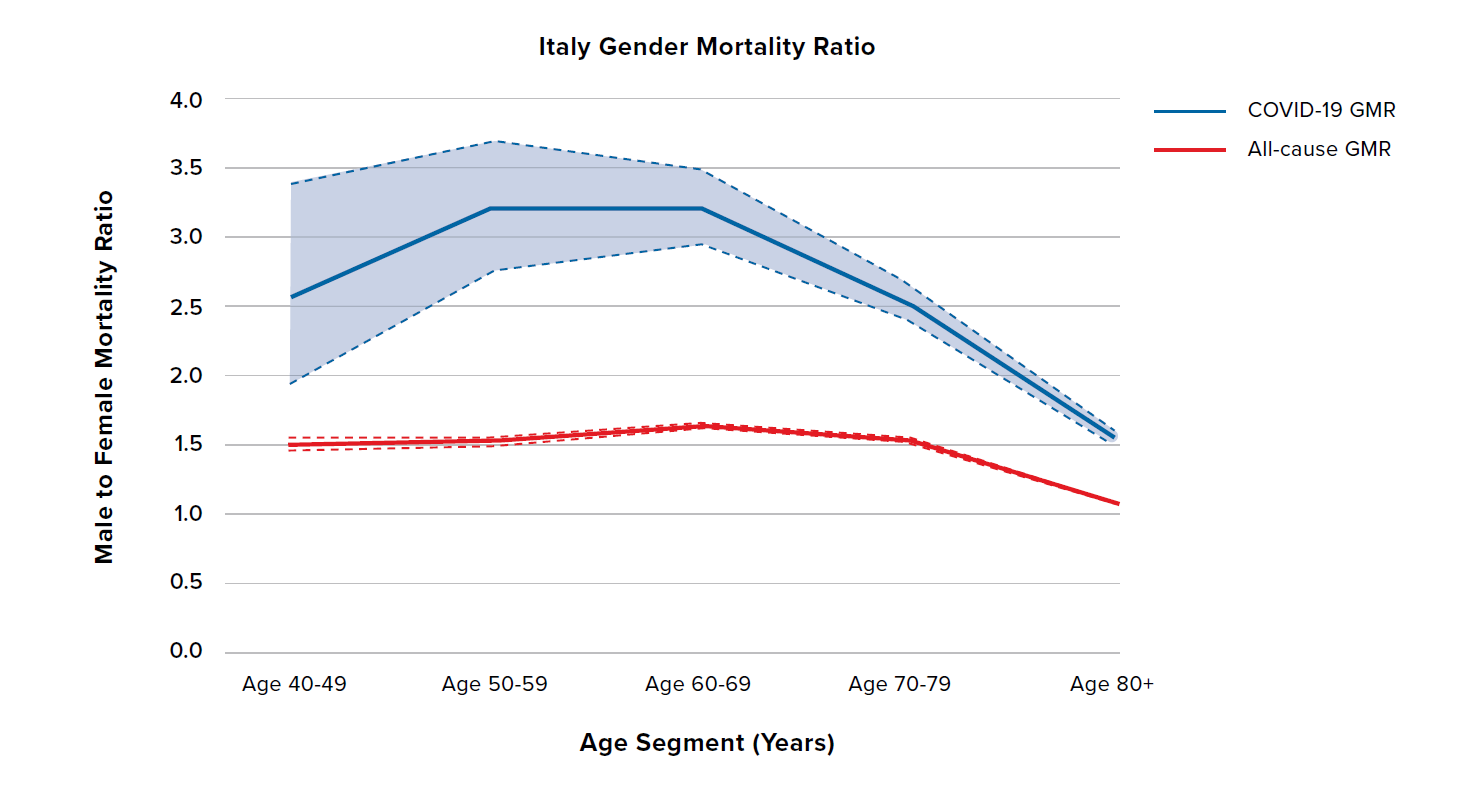
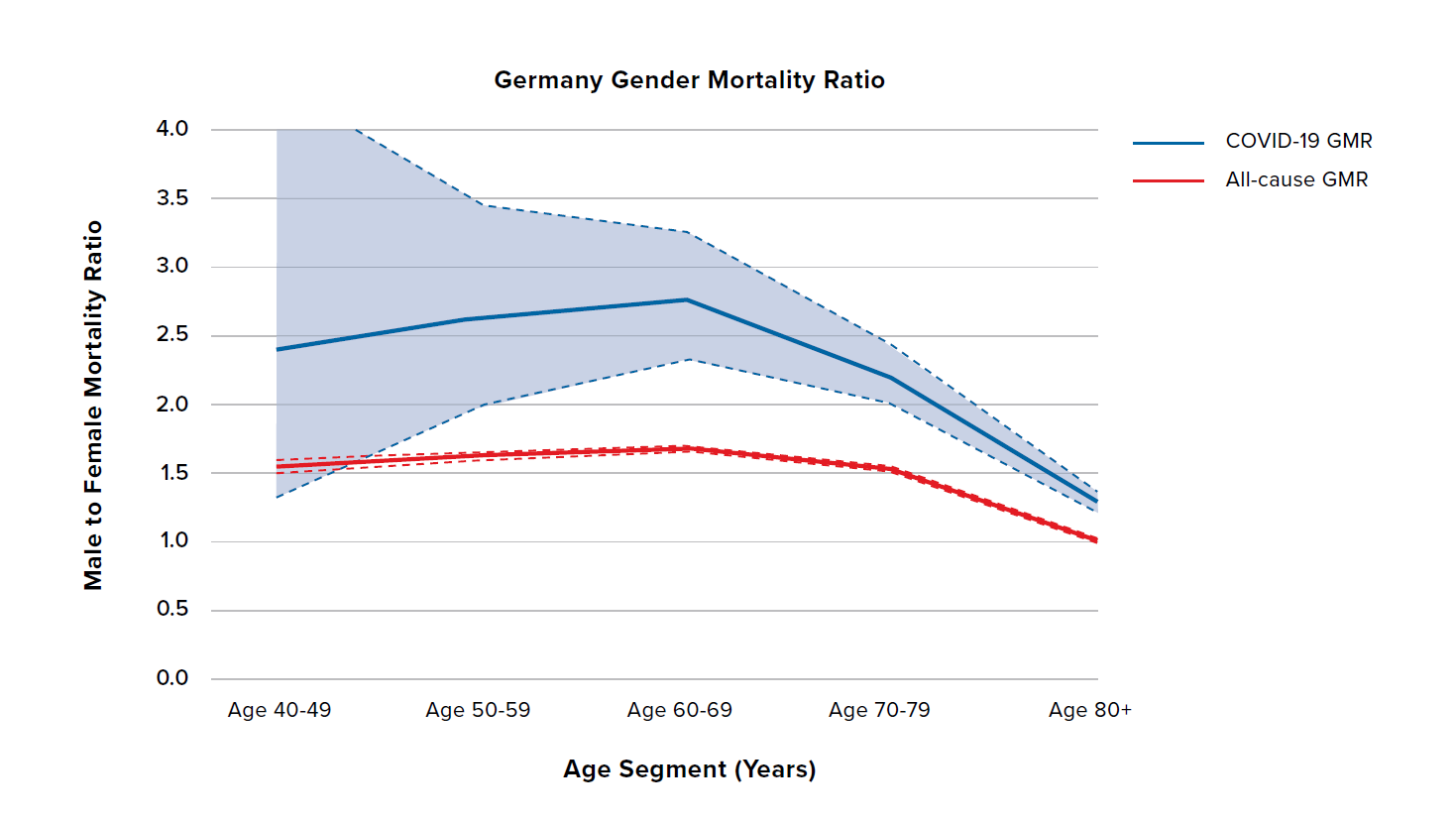
Figure 4 shows the COVID-19 and all-cause GMRs by age for Italy and Germany. The dashed lines and shaded regions represent 95% confidence intervals for each GMR. Italy and Germany have broadly similar all-cause GMRs. These two countries have the highest COVID-19 GMRs among the countries investigated, with male COVID-19 mortality 2.5 to 3.5 times that of females for all but the oldest age groups. Consequently, they also exhibit the largest gap between the COVID-19 GMR and the all-cause GMR – indeed, the sex difference for COVID-19 mortality is generally more than 2.0 times the sex difference seen in all-cause mortality.
Note the contrast in how Italy and Germany have experienced the pandemic so far. Some hospitals in Italy have been overwhelmed, with a high number of COVID-19 deaths, whereas COVID-19 mortality in Germany has been lower.
Figure 5 shows the COVID-19 and all-cause GMRs by age for the U.K., the U.S., Spain, and the Netherlands. The U.K., the U.S., and the Netherlands have relatively flat all-cause GMRs around 1.5, and COVID 19 GMRs generally between 1.5 and 2.5. The difference compared to all-cause GMRs is broadly similar and relatively constant across ages and countries. The exception is the Netherlands at ages 40 to 49, for which there is less data. Spain is broadly similar but with some potentially important differences: Spain has higher all-cause and COVID-19 GMRs with more of an inverted U-shape by age.
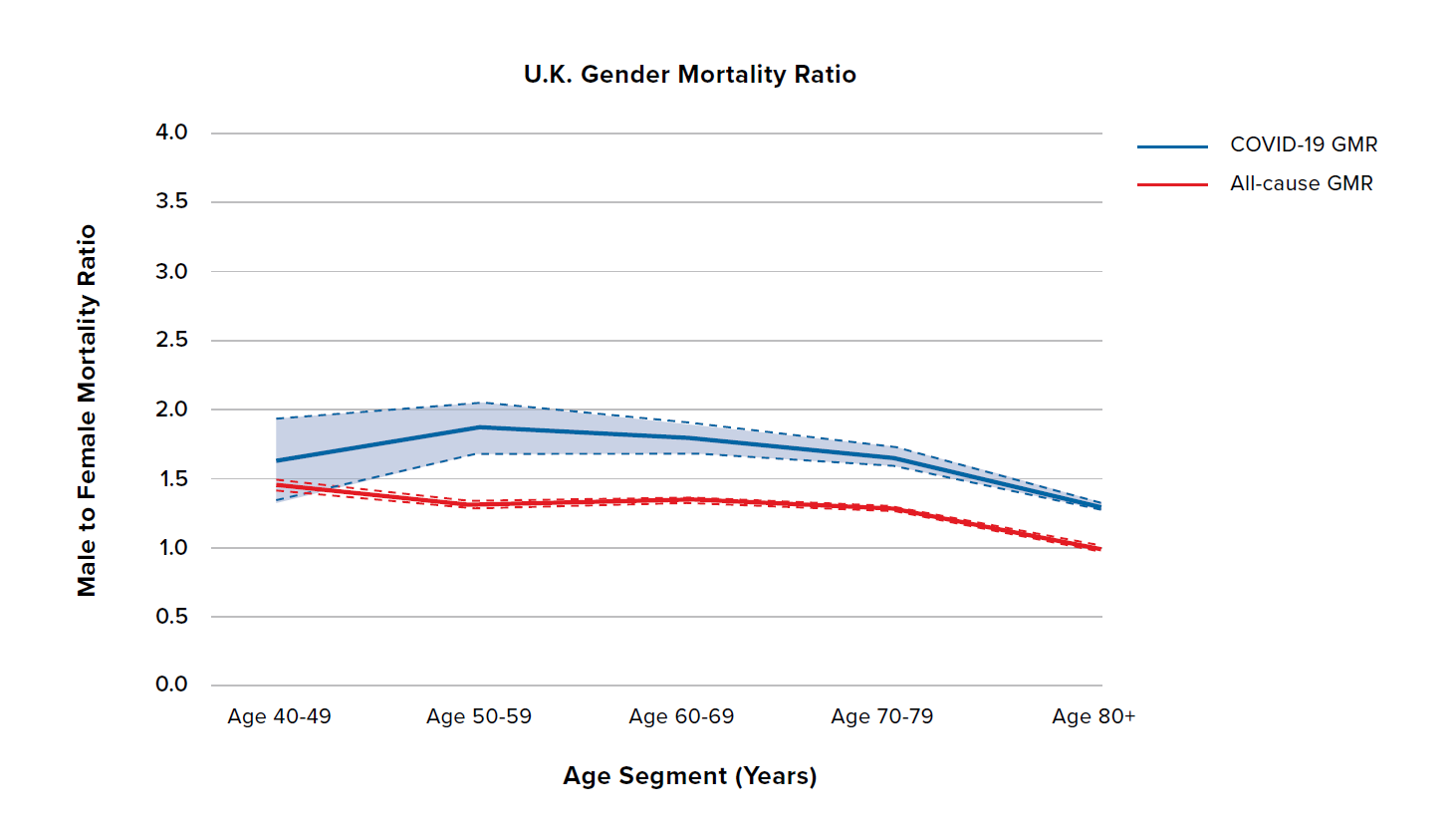
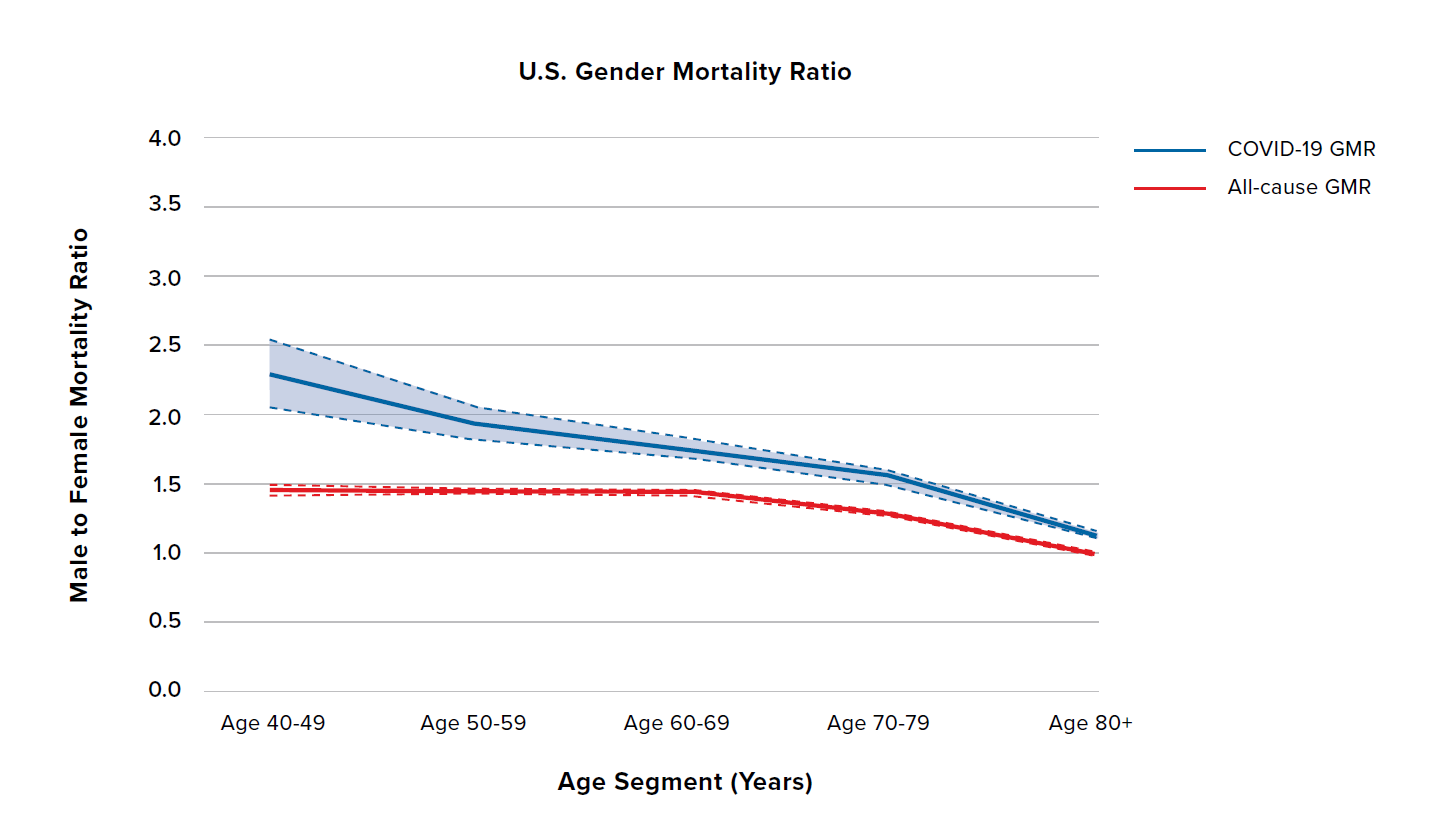
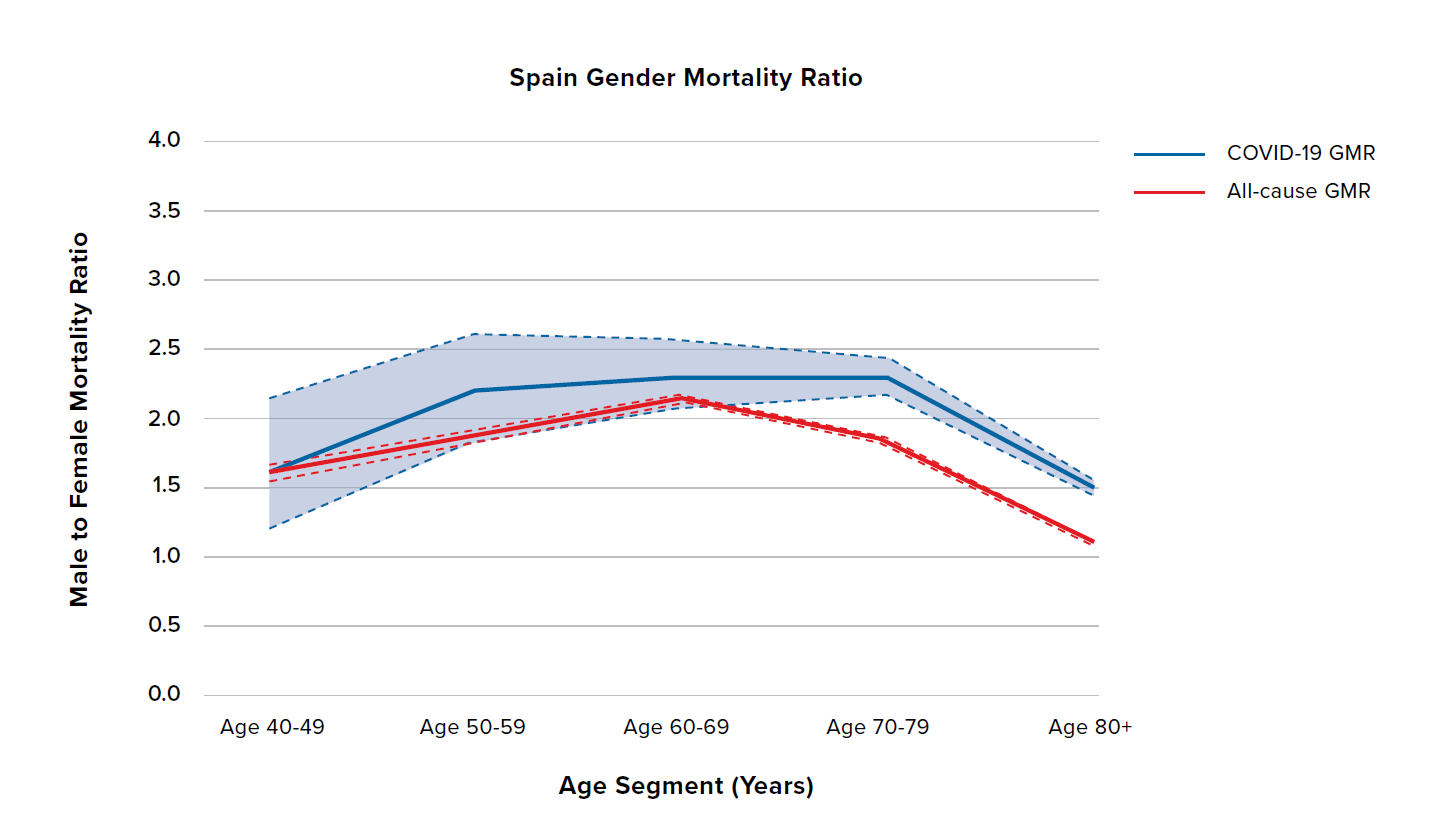
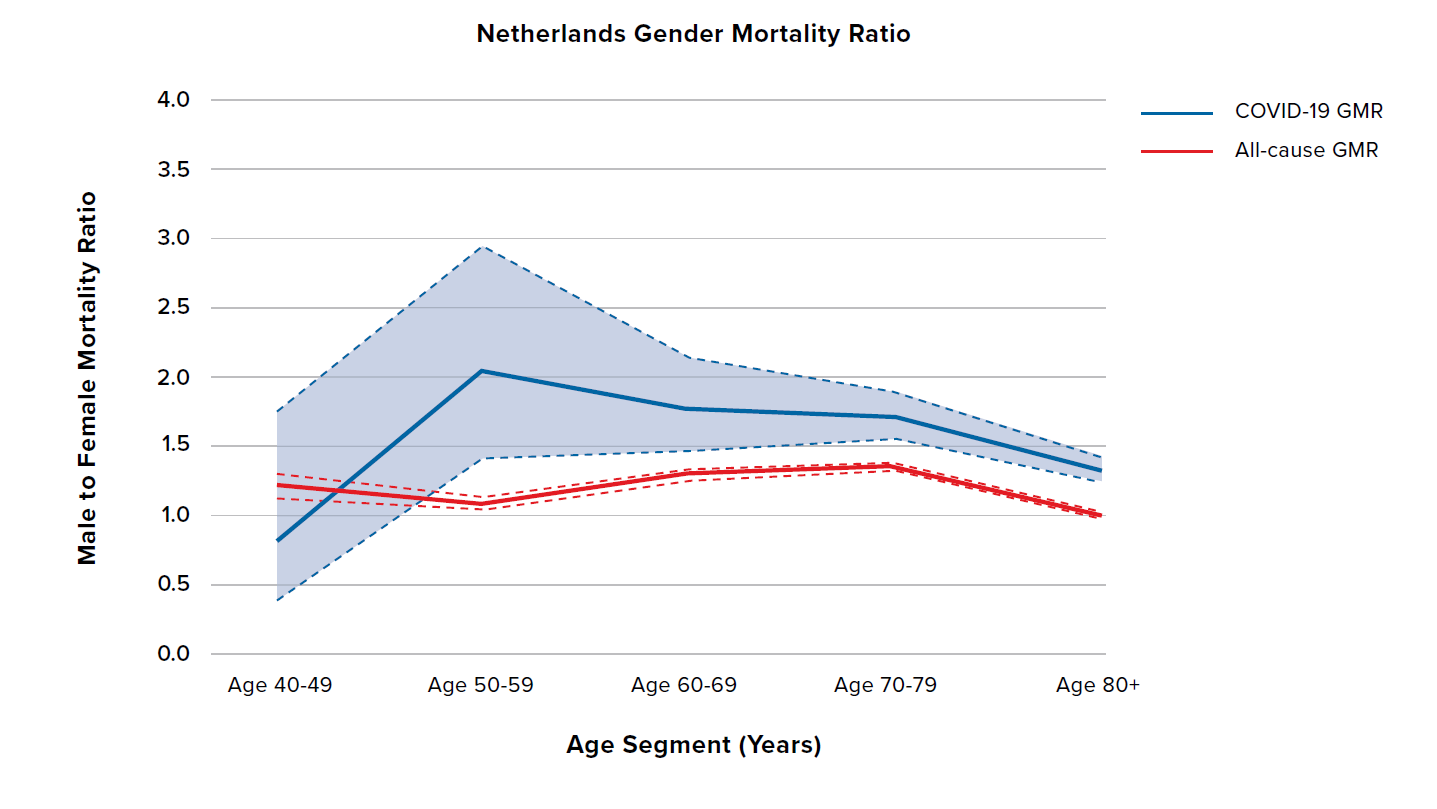
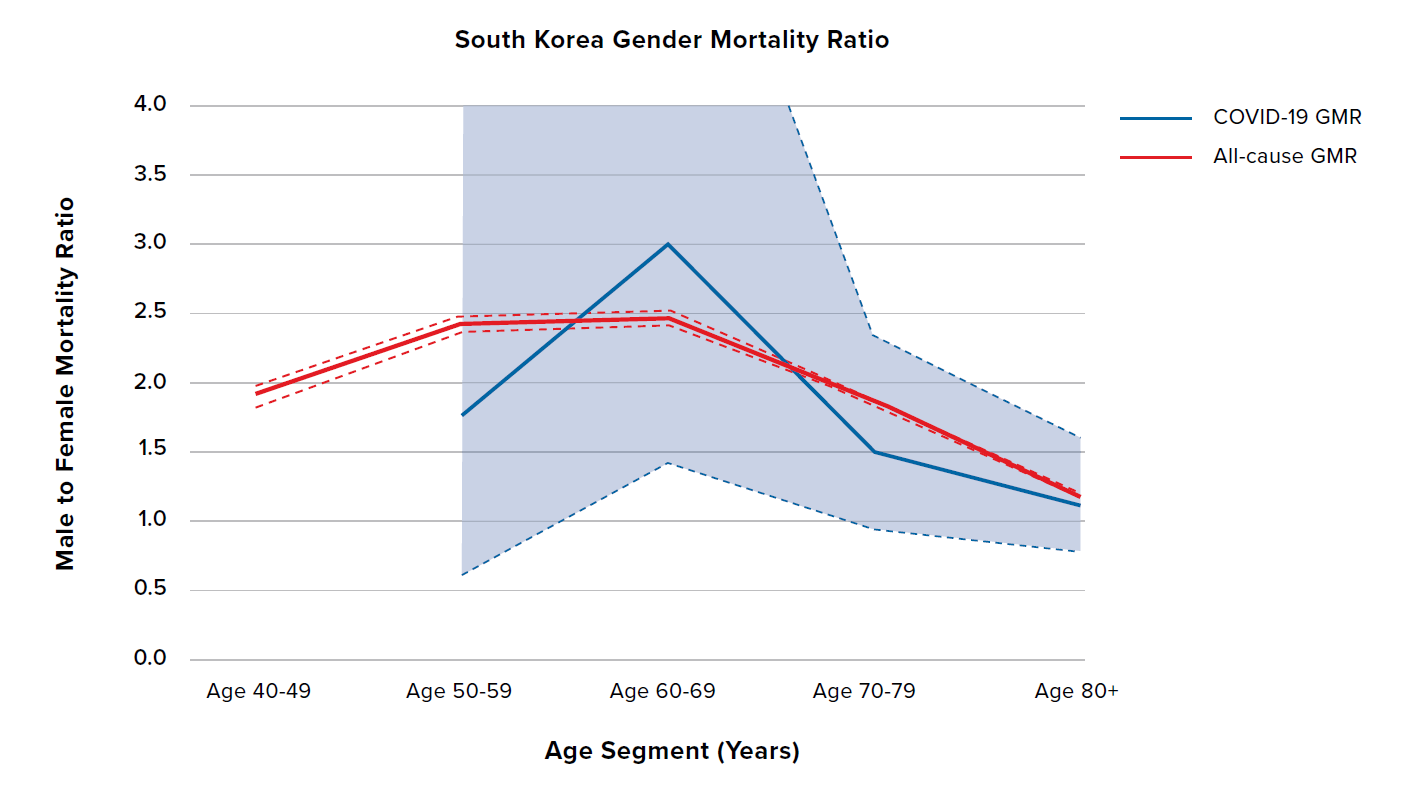
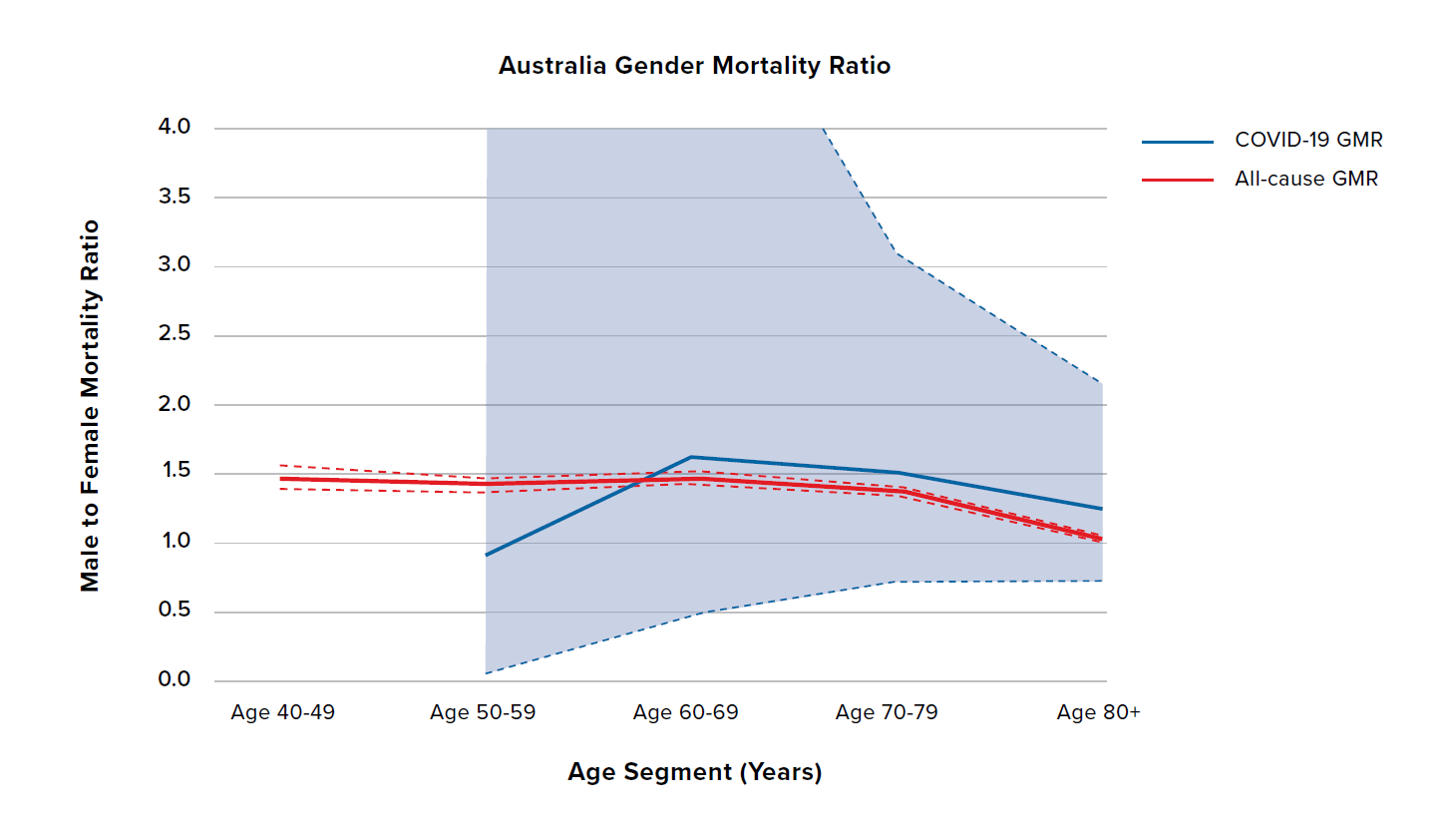
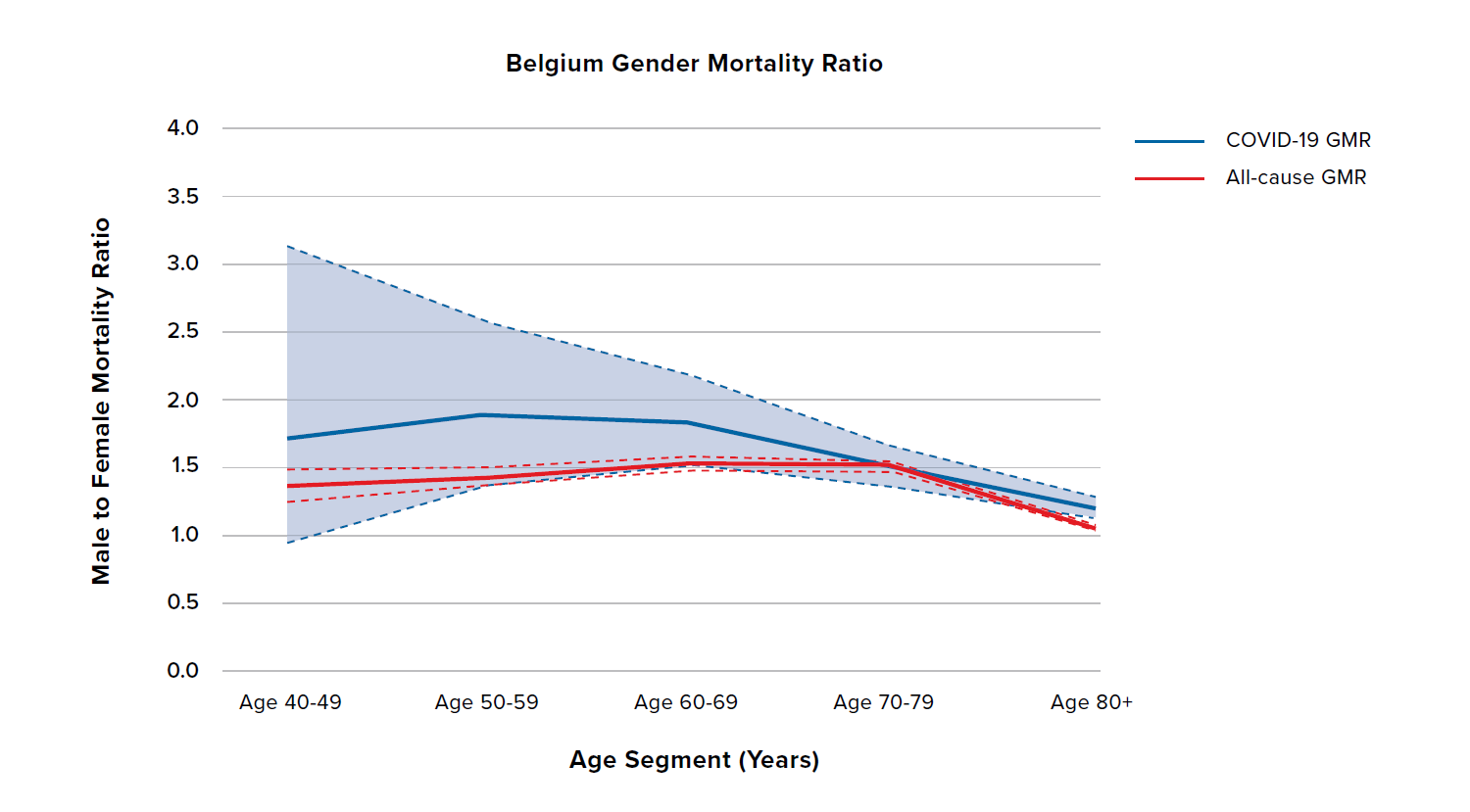
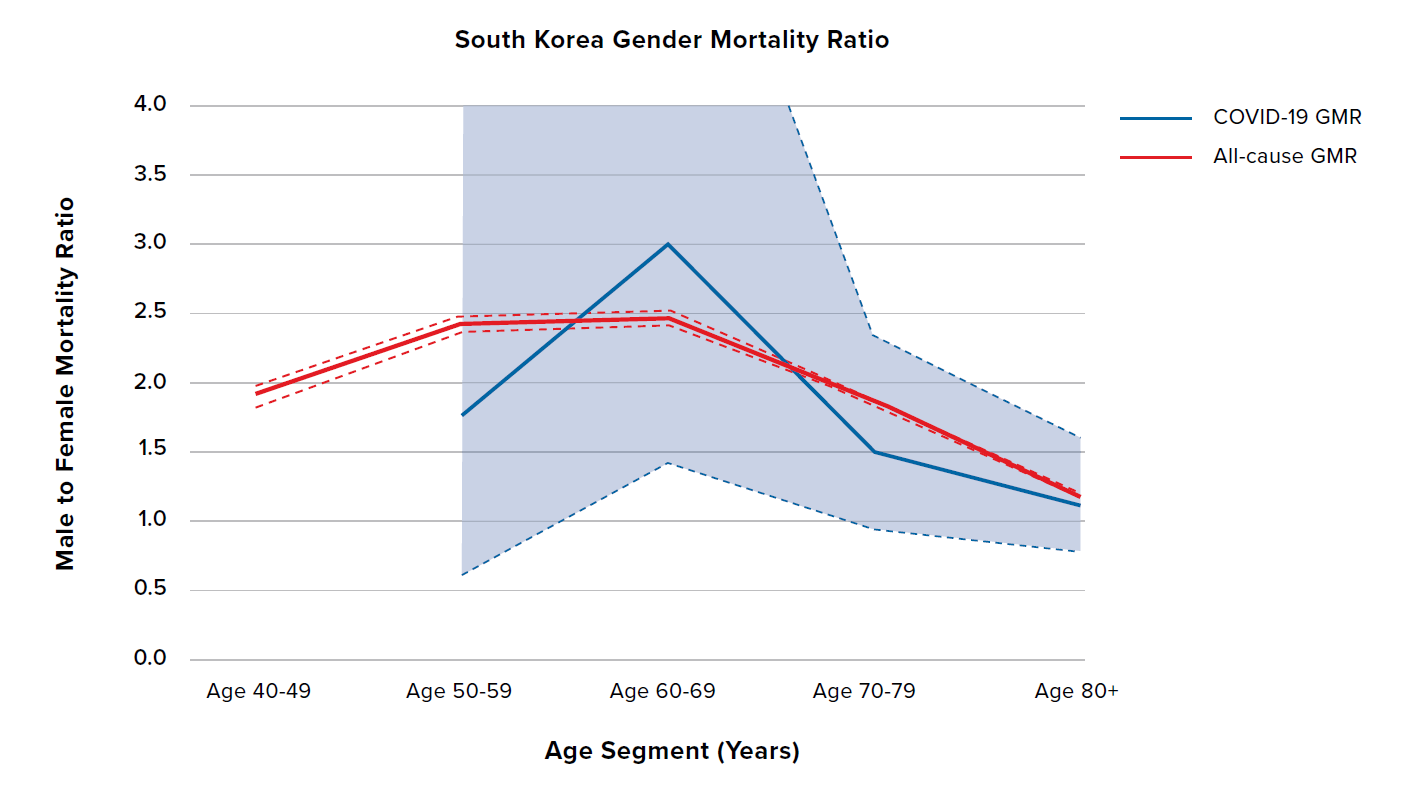
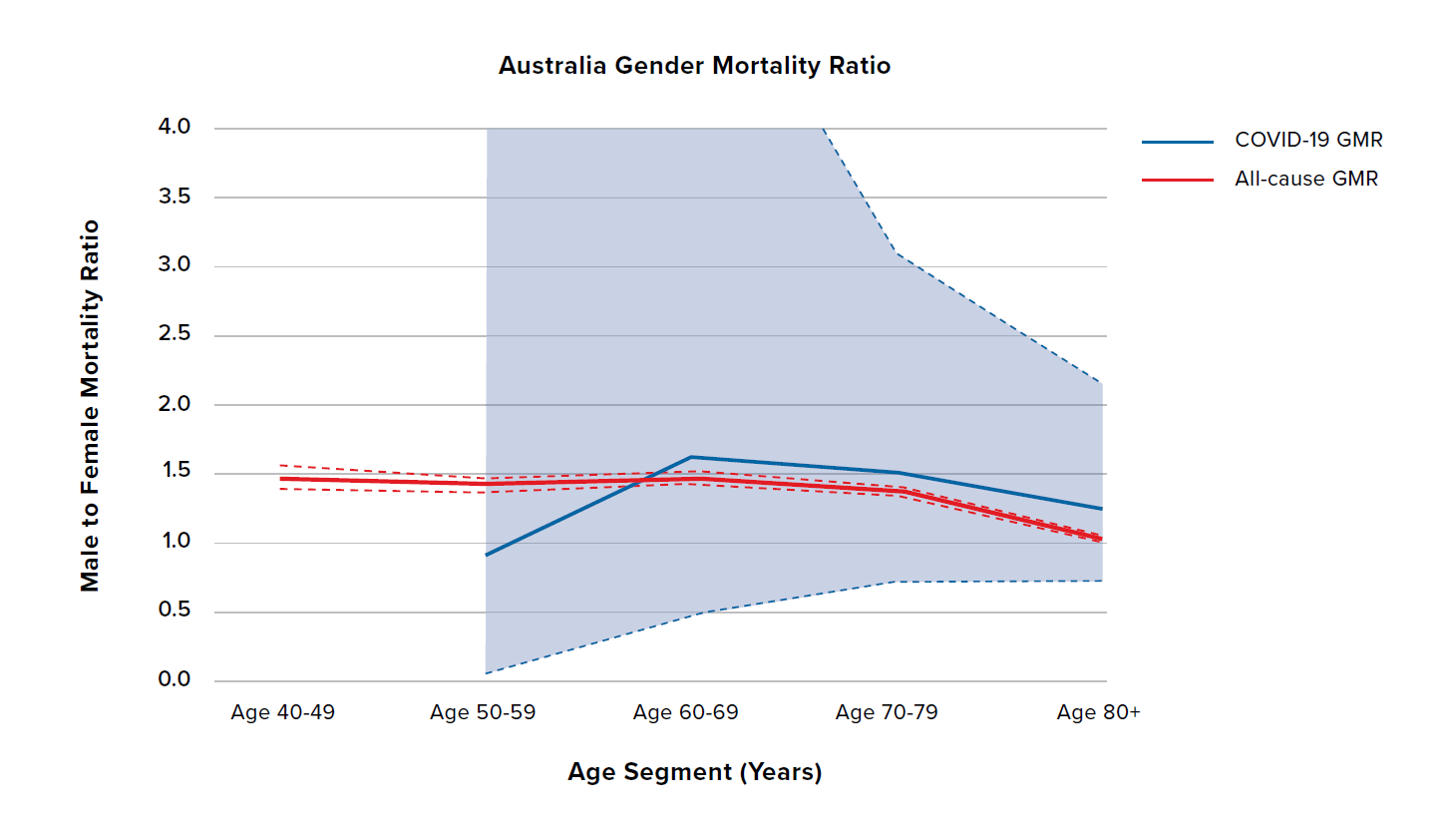
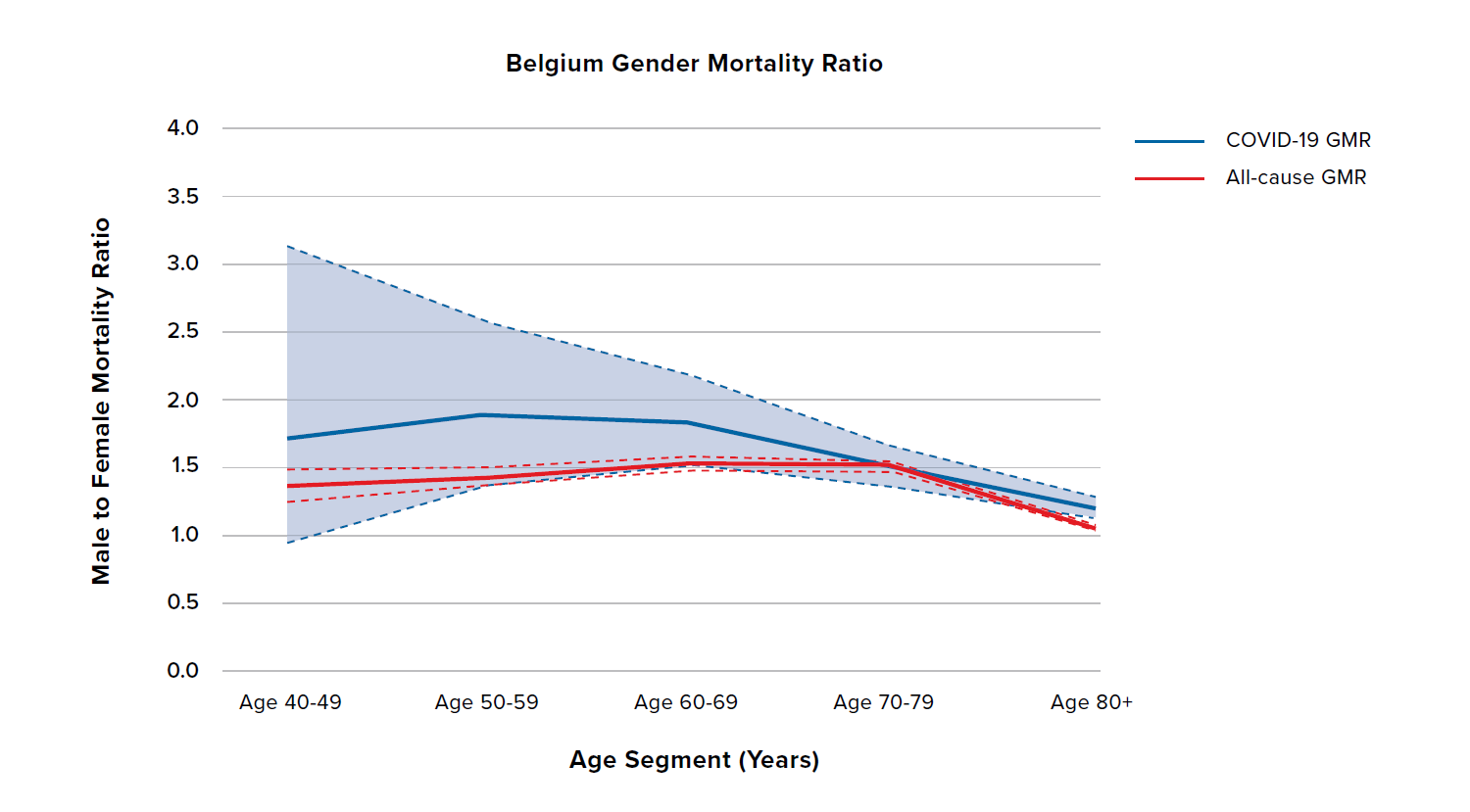
Figure 6 shows the COVID-19 and all-cause GMRs by age for South Korea, Australia, and Belgium. South Korea shows the highest all-cause GMR out of all nine countries, meaning that it already has a bigger difference in male and female all-cause mortality compared to the other countries. In addition, unlike the countries discussed previously, the COVID-19 GMRs for South Korea, Australia, and Belgium are broadly similar in terms of both level and shape to the all-cause GMRs. However, South Korea and Australia have experienced relatively low levels of COVID-19 mortality throughout the pandemic so far, which is reflected in the wide confidence intervals, so the results should be treated with caution.
Figure 6:
COVID-19 and all-cause GMRs by age in adults aged 40 years and older for South Korea, Australia, and Belgium
Discussion
This research report demonstrates how COVID-19 mortality rates differ by age and sex in nine countries. COVID-19 mortality exponentially increases by age for both males and females. The male COVID-19 mortality rate is generally higher than the female COVID-19 mortality rate across age segments in all countries. The age shape is broadly similar by sex within a country, although there are some differences between countries – for example, compare the mortality rates for males in Italy and the Netherlands.
Initially, smoking was thought to be one of the primary drivers of the sex difference in COVID-19 mortality risk. An elevated COVID-19 male death rate was first observed in data from China in February; a study of44,672 confirmed cases in Wuhan calculated the case fatality rate as 2.8% and 1.7% in men and women, respectively. Smoking prevalence in China is 52.1% among men and just 2.7% among women. In Italy, however, smoking rates are much closer between men and women – 28% of men are smokers, while 19% of women are smokers. This suggests that while the difference in smoking rates by sex is expected to be a contributory factor, it is not the critical factor explaining an elevated male death rate.
The variation in COVID-19 mortality is likely to reflect both sex differences (understood to mean the biological factors we associate with a person’s sex assigned at birth) and gender differences (taken to mean the combined effect of differences in social, political, legal, cultural, and economic norms). In terms of biological characteristics, it is well known that women produce stronger immune responses than men and are better at fighting off infection, including viral infection. The weaker male immune system leaves men more susceptible to a range of infectious diseases.
One potential explanation is that sex hormones are involved in the way the immune system triggers an inflammatory response to pathogens. Some researchers think these differences may also explain why men have been hit harder by COVID-19.
The SARS-CoV-2 coronavirus is closely related to the virus that caused the 2003 SARS outbreak. In SARS, more women than men suffered from the disease, but an analysis of all 1,755 cases in Hong Kong showed that the case fatality rate was significantly higher for men – 22.3% of males with the disease died compared with 13.2% of females. It is possible that differences in smoking prevalence may have contributed to this. However, research in mice infected with the SARS virus concluded that male mice suffered higher mortality, suggesting sex differences in the immune response were in some way accountable.
Angiotensin-converting enzyme 2 (ACE2), the host cell receptor that the SARS-CoV-2 coronavirus uses to invade human cells, might play an important role in in COVID-19 survival. Some researchers suggest gender differences in ACE2 expression levels may explain why more men are dying of the disease. Other researchers have suggested that the occurrence of ACE2 on the X chromosome could also drive worse survival in men – having only a single copy of the gene can enhance the harmful effects of X-chromosome-linked diseases.
In the current pandemic, we also see a higher number of confirmed cases in females compared to males in many countries. The table on the following page is taken from globalhealth5050.org. In Canada and many European countries, around 40-50% of confirmed cases are male (which means more female cases than male, similar to the 2003 SARS outbreak), while 50-60% of deaths are male (implying a higher case fatality rate for males).
In contrast, countries such as Peru, China, Pakistan, and Indonesia have more male cases than female, suggesting the possibility of testing bias or social and cultural gender differences in infection rates by country that are compounding the mortality difference by sex.
Table 1:
Data on total confirmed cases, deaths, and percentage of totals that are male, by country
Country
| Total Number of Confirmed Cases | Confirmed Cases (% male) | Total Number of Deaths | Deaths (% male) | Date Reported |
|---|
U.S. | 2,239,121 | NA | 103,337 | 54% | 17 Jun 2020 |
Peru | 257,447 | 58% | 8,223 | 71% | 22 Jun 2020 |
Spain | 248,335 | 43% | 20,527 | 57% | 21 May 2020 |
Italy | 238,050 | 46% | 33,209 | 58% | 16 Jun 2020 |
England | 228,742 | 43% | 37,664 | 57% | 17 Jun 2020 |
Germany | 190,431 | 48% | 8,880 | 55% | 22 Jun 2020 |
Mexico | 185,122 | 55% | 22,584 | 66% | 22 Jun 2020 |
Pakistan | 185,034 | 74% | 3,695 | 71% | 22 Jun 2020 |
Bangladesh | 115,786 | 71% | 1,502 | 77% | 23 Jun 2020 |
South Africa | 105,308 | 43% | 2,100 | 52% | 23 Jun 2020 |
Canada | 101,276 | 44% | 8,412 | 46% | 23 Jun 2020 |
Sweden | 60,837 | 41% | 5,161 | 55% | 23 Jun 2020 |
Belgium | 60,567 | 37% | 7,016 | 51% | 19 Jun 2020 |
China | 55,924 | 51% | 2,114 | 64% | 28 Feb 2020 |
Netherlands | 49,631 | 38% | 6,095 | 55% | 23 Jun 2020 |
Indonesia | 47,896 | 53% | 2,535 | 61% | 23 Jun 2020 |
Argentina | 42,785 | 51% | 1,016 | 57% | 22 Jun 2020 |
Columbia | 40,719 | 55% | 1,308 | 61% | 08 Jun 2020 |
It is possible that behavioral differences as simple as compliance with handwashing advice could also play a part in infection rates.
In this report, we compared COVID-19 GMRs against all-cause GMRs to determine if the sex difference in COVID-19 mortality is greater than in all-cause mortality. The sex difference in COVID-19 mortality was observed to be greater and to have a bigger variation than the sex difference in all-cause mortality, although part of this may be due to low data volumes at some ages in some countries.
At ages 80 and older, where COVID-19 death data is relatively more abundant and hence more credible, we saw some level of convergence in COVID-19 GMRs across countries, at around 1.2 to 1.9. This is slightly higher than the level at which the all-cause GMRs converge (1.1 to 1.3).
We split results into country groupings; the GMR results are summarized below. South Korea and Australia have low data volumes, so their results should be treated with caution.
Countries | Ratio of male to female COVID-19 mortality | Comparing COVID-19 GMRs to all-cause GMRs |
|---|
Italy, Germany | 2.5-3.5x | 2.0x |
U.K., U.S., Spain, Netherlands | Around 2.0x | 1.3x |
South Korea, Australia, Belgium | 1.5-3.0x | Similar |
Trends in COVID-19 mortality rates will change as the pandemic progresses, due to such factors as relaxation of mitigation measures and other government strategies. RGA continues to monitor the emerging data. The varying COVID-19 mortality rates by age, gender, and country illustrated in this paper also reflect differences in population health, lifestyle behaviors, and sociodemographic factors, as well as government policies. We hope to include other stratifiers of risk in future reports if the data are available.
A number of research studies have started to explore multivariable associations with COVID-19 mortality. For example, in a U.K. study, male sex remained a significant predictor for risk of dying from COVID-19 (hazard ratio equal to 1.99, which is remarkably similar to what we observe) after controlling for age, BMI, smoking, ethnicity, socioeconomic status, and underlying health conditions. Other research, also based on multivariable models of risk, has demonstrated higher mortality risk for males in U.K. hospitals. In addition, recent research suggests that susceptibility to SARS-CoV-2 infection is also dependent on sex, with men having an odds ratio of approximately 1.55 compared to women.