As more countries either partially or fully legalize cannabis for medical or recreational use, underwriters should be aware how changes in legislation may affect disclosures by applicants regarding their use of cannabis.
This article explains the different types of cannabis products available, discusses how increasing cannabis potency is impacting cannabis users, and takes a look at current cannabis legislation around the world.
What’s what?
Cannabis (common hemp/ditchweed) is a flowering plant from the Cannabaceae family, which consists of three primary species: Cannabis sativa, Cannabis indica, and Cannabis ruderalis.1 Herbal cannabis, better known as marijuana, consists of the dried flowers and leaves while cannabis resin is made from the resinous parts of the plant, which include compressed or purified preparations of stalked resin glands, called trichomes. The main active ingredient in marijuana is tetrahydrocannabinol (THC), a cannabinoid, which is responsible for giving a person a feeling of euphoria, or ”a high,” with THC concentrations being much higher in resin than herbal cannabis. A number of cannabis strains have been cultivated to either lower or raise the THC content of the plant in order to make different compounds or satisfy narcotics legislation.2
Cannabidiol (CBD) is a cannabinoid derived from the flowers of the cannabis plant and is used to help alleviate adverse symptoms of cancer, weight loss in AIDS, chronic pain, spasticity, seizures, glaucoma, arthritis, and migraines. Unlike THC, CBD is not associated with addiction and is not a psychoactive ingredient. On this basis, many U.S. states have legalized CBD but not marijuana.
…and what’s important
New cultivation methods have created hybrid plants which yield greater THC, and these plants are now replacing many common cannabis varieties around the world. Different strains of the cannabis plant can produce very different effects based on their THC to CBD ratios, and many consumers of cannabis products are not aware of either the THC or CBD content. In the U.S., cannabis products sold legally have to be tested for THC and CBD content and labelled accordingly.3
It is common for dispensaries in the U.S. to sell concentrated cannabis products with THC potency up to four times the strength of what is typically found in smoked cannabis. The Colorado Department of Revenue reported that in 2015, dispensary-sold flower strains had an average THC strength of 17.1% but that the average strength in concentrated cannabis products was 62.1% THC. Furthermore, sales of concentrates more than doubled between 2015 and 2016.4 The increasing popularity of concentrates is clearly of concern, particularly when assessing the potential long-term health risks.
Only a limited number of studies have compared the effects of smoked versus vaped cannabis, but a study by Spindle et al found that vaporised cannabis produced stronger drug effects and higher peak concentrations of THC compared with equal doses of smoked cannabis.5
A study examining the changes in cannabis potency in the U.S. over the last two decades found that from a sample analysis of 38,681 cannabis preparations seized by the U.S. Drug Enforcement Agency (DEA) between 1995 and 2014, overall THC potency of illegal cannabis had risen from 4% in 1995 to 12% in 2014. Conversely, CBD was found to have fallen in strength from 0.28% in 2001 to <0.15% in 2014, resulting in a ratio change in THC to CBD content from 14 times in 1995 to nearly 80 times in 2014. The study further found that in U.S. states where cannabis was legal, the average THC concentration was 8.73% (+ 6.08%), but in U.S. states where cannabis was not legal, THC strength was 5.42% (+ 4.9%).6
A 2019 study published in The Lancet reviewed the risk of later psychotic disorders in cannabis users across Europe. The study noted that daily cannabis users had a threefold to fivefold increase in the risk of psychosis. A fivefold risk of psychosis was found in individuals who consumed cannabis products with a THC potency of >10%.7
Prevalence
Cannabis is the world’s most commonly used drug and the most commonly used illegal drug in Europe. In 2017, there were an estimated 188 million cannabis users worldwide. The number of people using cannabis continues to rise, with the global number of users increasing 19% from 2009 to 20178
According to the European Drug Report 2019, nearly a fifth of all 15-24 year olds admitted using the drug in the last year. User prevalence ranged from 3.5% in adults aged 15-34 in Hungary to 21.8% in France. Increasing consumption trends have been found in a number of European countries such as Finland and Ireland, and an estimated 1% of adults in the European Union consume cannabis on a daily basis or have consumed cannabis on 20 days or more within the last month. The vast majority (60%) are under age 35 and are male. 9
The 2013 U.S. National Drug Strategy Household Survey report found that cannabis use by adults age 21 and over appears to have increased following the legal use of cannabis for medical purposes, but no difference in prevalence was found in U.S. states where the medical use of cannabis was legalized and those where it was not. However, in states where cannabis was legalized for medical use, adults were more likely to have used cannabis in the last 30 days, more likely to be daily cannabis users, and were more likely to report symptoms of dependency.10
Cannabis Products
Numerous cannabis-based products are available for purchase in different forms, such as dried cannabis, oils, edibles, liquids, and creams. Edibles include products such as chocolate, biscuits, and jellies, and concern is growing about the sale of extremely potent edible products. The effects from edibles containing THC can take up to 60 minutes to be felt, increasing the risk of consuming too much of the product.10
Changes in legislation are driving other innovative products such as low THC strength cannabis oils, which are available for sale in health food shops and related establishments. Many of these products claim to have less than 0.3% THC and are aimed at either cannabis smokers or those who use cannabis for health and well-being.9 Pure CBD oil contains less than 0.2% of TCH and therefore has no psychoactive component. Following the recommendation by the World Health Organization (WHO) Expert Committee on Drug Dependence, the United Nations (U.N.) is waiting to take a vote on CBD preparations containing not more than 0.2% THC, in order to remove them from international drug control as they do not have psychoactive properties and, as yet, no cases of drug dependence reported.10,11
Medicinal Cannabis
Very few reliable studies or sizeable clinical trials completed to date examine the effects of cannabinoids on humans, either for medicinal or recreational purposes. Dronabinol (Marinol) was approved in the U.S. in 1985 to help patients with nausea and vomiting as a result of cancer chemotherapy, while Syndros (liquid dronabinol) was approved in 2017. Nabilone, sold under the brand names Cesamet (approved in 1992) and Canemes, is used to help alleviate adverse symptoms experienced by chemotherapy and AIDS patients.
Clinical trials for nabiximols (Sativex), available in most European countries, showed only marginal improvements in muscle spasticity for many patients with multiple sclerosis (MS). Parents of children with severe epilepsy report that CBD oil (Epidiolex) significantly reduced seizures in children with Dravet syndrome or Lennox-Gastaut syndrome. However, the strength of any evidence supporting the use of cannabis in multiple conditions to date is either weak or moderate.10
Cannabis and the Law
Uruguay was the first country to fully legalize cannabis in 2013; Canada and Georgia followed suit in 2018. Other countries have only decriminalized cannabis or allowed for its medical use. The medical use of cannabis for specific conditions has been legalized in a number of countries, including Israel (2001), the Netherlands (2003), Switzerland (2011), Australia (2016), and Germany (2017).10 In 2018, South Africa legalized the private use, cultivation, and possession of cannabis for personal consumption. Portugal decriminalized cannabis possession in 2001 for amounts of up to 25g, while Spain and the Netherlands allow for cannabis to be consumed in special cannabis shops and clubs. Other countries, such as Norway and New Zealand, are considering legalization of cannabis.12, 13
Medicinal cannabis remains illegal in Cambodia, Japan, Nepal, Pakistan, and Vietnam. The Philippines has approved cannabis for medical use, while Thailand is currently proposing to reclassify marijuana as legal for medical purposes. 14 Australia legalized the use and production of medical cannabis in 2016 but prescriptions may only be issued by an oncologist, neurologist, or pain specialist and can only contain a maximum of 2% THC.10 New Zealand’s regulations have allowed for prescription CBD by a doctor since 2017.15 In the U.S., given that legislation is considered at both a federal and a state level, cannabis laws vary significantly from state to state, and legislation around cannabis is further complicated by DEA and Food and Drug Administration (FDA) oversight. While the maximum THC content in the U.S. has not been set, Canadian regulations state that “maximum THC content in dried cannabis consumed by inhalations must not exceed 1g in each discrete unit of cannabis product” and that those products taken orally, rectally, vaginally, or topically “must not exceed a maximum yield quantity of 10mg of THC.” 8
Risks from Cannabis Use
It is difficult to establish the true risk of adverse mental and physical health effects of using different forms of cannabis. Large variations in amounts of THC and CBD exist within products, and different risks stem from the way the product is consumed and the frequency and duration of consumption.
A number of studies found the lifetime risk in the early 1990s of developing a cannabis dependency in the U.S. was 9%, compared with 32% for nicotine, 23% for heroin, 17% for cocaine, 15% for alcohol, and 11% for stimulants. Certainly, long-term cannabis smoking increases the risk of chronic bronchitis, and about 70% of those who use marijuana also smoke tobacco.16 Many cannabis users now take it in capsule form or other non-smoking method. Other risks associated with the long-term use of cannabis include an increased likelihood of progressing to other illicit substances such as cocaine. 10
Morbidity risks include an increased risk of cardiovascular disease, chronic bronchitis, impaired cognitive development, and mental health issues, particularly in adolescents. Emergency department visits by adolescents aged 15-17 who have consumed cannabis have risen in the U.S. in both males and females, by 53.6% and 42.9% respectively, from 2005 to 2010.6 According to the Substance Abuse and Mental Health Services Administration (SAMHSA), children who consume marijuana have a fourfold risk of becoming a heavy chronic user.17
However, studies have not yet found a relationship between marijuana use when consumed in lower doses and psychiatric disorders. If consumed in higher doses/potency or with regularity, some studies note that marijuana use could lead to exacerbation of existing psychiatric conditions.18, 19
Underwriting Considerations
For insurance underwriting purposes, individuals consuming cannabis prescribed by a legally authorized physician and/or authority for a specific cause/disease/impairment and through legally authorized dispensaries should be considered medicinal cannabis users. Individuals buying it over-the-counter or with self-defined medical marijuana use for health and well-being should be considered recreational cannabis users. Risk factors such as the method of consumption, the reasons for use, and the type, frequency, and duration of cannabis consumption should be considered at the underwriting stage. RGA’s findings indicate that the increasing strength of cannabis products and the ratio of THC to CBD are of considerable concern. Also a concern is the number of occupations noted to have higher prevalence of marijuana use.
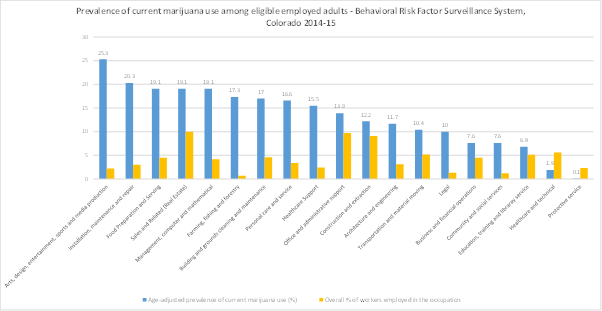
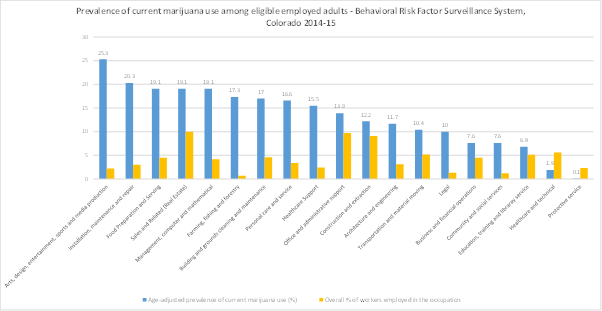
A report published by the U.S. Centers for Disease Control and Prevention (CDC) highlights a high number of marijuana users working in the arts, entertainment, and the recreation industry, as well as in the accommodation and food services industry. The chart below shows the occupations with highest prevalent use of marijuana among employed adults.
Figure 1. Prevalence of current marijuana use among eligible employed adults (n=10,169), ranked by occupation, and overall percentage of state workers employed in the occupation – Behavioral Risk Factor Surveillance System, Colorado, 2014-15. The blue bars indicate the occupations with percentage prevalence and the yellow bars indicate the percentage of state workers employed in the occupation. 20
For individuals using medicinal marijuana, underwriters should request all details about any underlying disorder, including its chronicity, severity, and treatment regimens. One needs to always remember that cannabis is not a first line therapy nor a curative therapy for most medical disorders, but is used as an adjunct therapy or for palliative purposes only.
Conclusions
Regardless of whether cannabis has been legalized in the country where an applicant has applied for insurance, the focus should be on disclosures regarding the amount, frequency, and duration of use; product type and method of consumption; and especially the THC strength and THC/CBD ratio in products consumed. The use of edibles or CBD oils presents new challenges, as do rapidly changing markets amid new legalization. While the long-term consequences of consuming today’s cannabis products are as yet unknown, the insurance industry must proceed with caution when underwriting such risks, regardless of legal status.