Impacts of Gene and Cell Therapies
Since the emergence of gene therapy as a treatment category, several gene therapies have been successfully developed and granted approval by the Food and Drug Administration (Table 3). Even more gene therapies are in the pipeline and will likely be approved in the near future.
These therapies typically cost millions of dollars per dose or course of treatment. Billing for these treatments has been under J-Codes thus far, and so they generally fall under Medicare Part B coverage.
As some gene therapies are specifically for children (e.g., Zolgensma, Skysona, Elevidys), Medicare, Medigap, and MA plans are not expected to experience the full cost impacts of these therapies. That said, many gene therapies are indicated for conditions for which persons under age 65 can enroll in Medicare through meeting its disability eligibility rules. These conditions include, but are not limited to, retinal dystrophy, spinal muscular atrophy, Duchenne’s muscular dystrophy, dystrophic epidermolysis bullosa, and sickle cell anemia. Thus, Medigap and MA insurers are and will be subject to some financial risk from people both over and under age 65.
Cell therapies, costing hundreds of thousands of dollars per person per year for the treatment of blood cancers, are also available. Expensive solid tumor cancer cell therapies are expected to be approved in the near future. All of these are bound to generate higher financial risks for Medigap and MA plans.
While manufacturers have yet to meet the high demand for cell therapies now available, they are working hard to find efficiencies that might make these solutions more widely available. Table 4 lists commercially available cell therapies as of February 2024. One of them, Lantidra, treats type 1 diabetes, while the rest treat certain blood cancers – including multiple myeloma, leukemia, and lymphoma – and melanoma. Manufacturers are also seeking to gain FDA approval for use of cell therapies for people with earlier-stage cancers.
Manufacturer prices for cell therapies are between $300,000 and $500,000 per treatment for Medicare enrollees. However, that is not the full extent of the financial risk to Medigap and MA plans. There are also significant hospital and physician charges associated with the delivery of these treatments. Total costs of cell therapies can typically range anywhere from $600,000 to $1.2 million, with higher costs experienced at more expensive facilities or when adverse patient safety events occur. Medigap would cover Part A’s deductible and up to 20% of the Part B coinsurance charges.
There are material emerging risks for Medigap insurers for which the use of reinsurance should be considered. These include high-cost specialty drugs covered in Part B and the growing number and type of gene and cell therapies.
Impact of Baby Boomers Entering Retirement
The aging of the baby boom generation into Medicare eligibility, while a major program cost inflator for CMS and the U.S. health system overall, is also working out to be a short-term cost deflater for Medigap and MA, at least on a per-person basis. While this may at first seem counterintuitive, over time, the influx of boomers into Medicare’s ranks may yield reduced average claim numbers in the short term, due to a younger average age of enrollees. It will, however, likely have an opposite impact as this generation ages further.
That said, there are major state-by-state differences in how Medigap rates are allocated by age. These differences play a large role in how rates work in practice in any given state and for any given insurer. For example, Medigap insurers often make individual rate increase requests for specific pooled cohorts, such as groups pooled by the year in which the policies were sold or groups pooled by plan type. When mixed with differences in state oversight on rate requests for these cohorts, there can often be a wide range in Medigap rates, even within a given state.
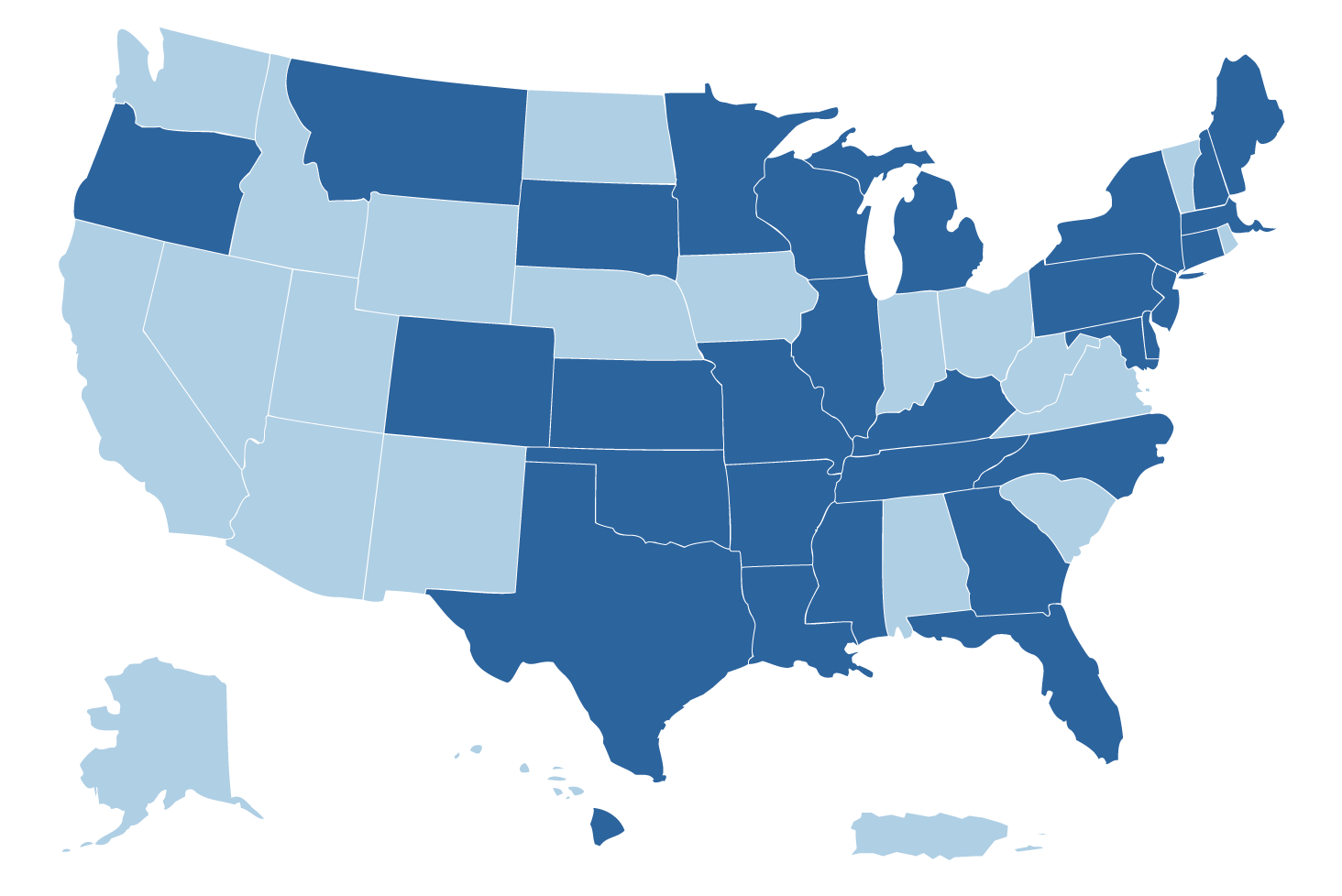
Diving deeper into age-rating differences in Medigap, it is important to understand that most states are “attained-age-rated,” meaning that annual rate increases are affected both by health care cost inflation and enrollees being one year older.
Four states (Arizona, Florida, Georgia, and Idaho) are “issue-age-rated,” which means the age at initial issuance of the Medigap policy will drive the initial rate, and future rates will be driven mainly by common health inflation-driven rate increase requests from the insurer (but not the enrollee’s current age).
Medigap plans in eight states – Arkansas, Connecticut, Maine, Massachusetts, Minnesota, New York, Vermont, and Washington – as well as MA plans nationwide are community-rated (or “no-age-rated”). This means neither the insured’s age at issuance of the policy nor their current age affect the rate. Every purchaser pays the same fundamental rate for each product, although there can often be rate differences for variables such as smoker status and geographic locations. In community-rated plans, health inflation as well as a pool’s claims experience will affect whether enrollees in these plans have an annual rate increase, and if so, the amount of the increase.
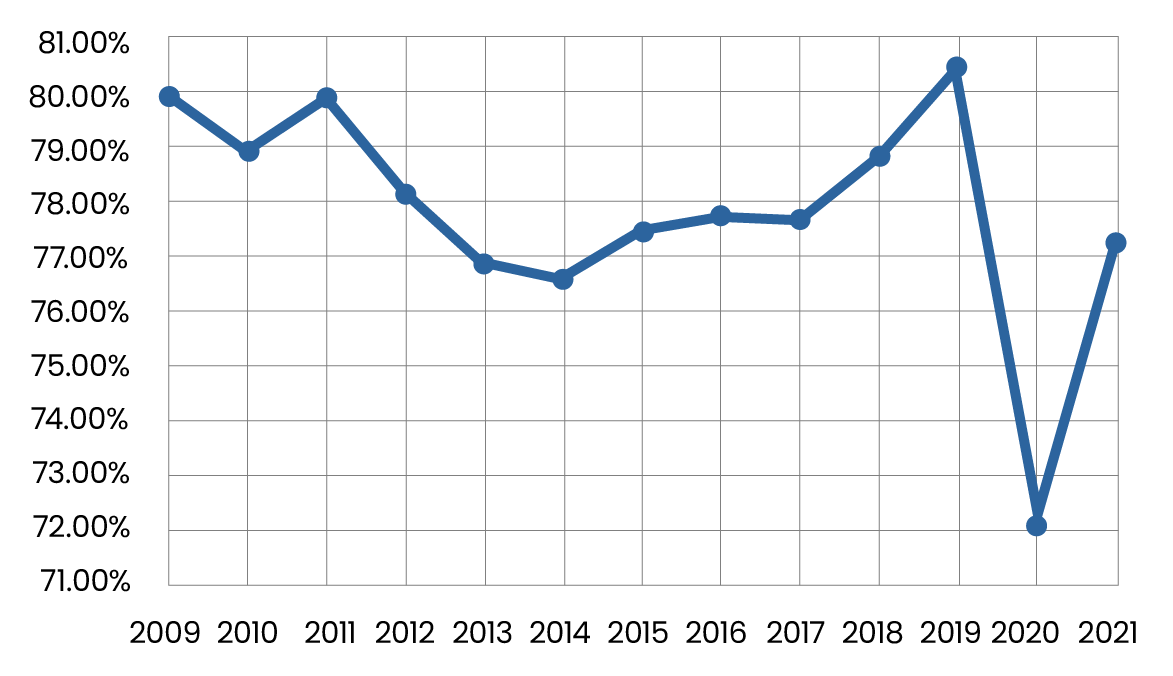
Because average medical costs increase with age, the aging of baby boomers into Medicare eligibility has been particularly advantageous for community-rated and issue-age-rated Medigap plans. The average age of the Medicare population is decreasing as more and more baby boomers turn 65 and enroll in Medicare or MA. MA rate increases have also been relatively low compared to industry expectations over the last decade, at least partly due to this phenomenon. A December 2019 study by The Commonwealth Fund estimated that the influx of baby boomers into traditional Medicare (though not MA plans, which were excluded from the study) reduced the program’s health inflation by about 0.84% per year from 2007 through 2015.6 While policy experts and health economists often comment on this trend influence as small and immaterial, most health actuaries would disagree.
Medigap Competition with Medicare Advantage
The Medicare Advantage share of the Medicare market has grown significantly over time, from 19% in 2007 to 50% in 2023.7 This growth has cut into Medigap’s market share (though not overall enrollment counts), as coverage under both policy types is not permitted (an administrative check at enrollment ensures this). This market share impact is driven mainly by three factors: advantageous payment streams from the Centers for Medicare and Medicaid Services (CMS) to MA plans relative to the payment streams from MA plans to providers; quite a bit of advertising; and the MA plans’ ability to flexibly enhance coverage beyond the standardized Medicare coverage.
In terms of the last point, many states do not let Medigap insurers provide benefit coverage enhancements – such as dental, vision, hearing, and wellness – that MA plans have the flexibility to offer. Even in states that allow Medigap plans to offer certain optional enhancements, some require that those enhancements be renewed annually throughout the enrollees’ lifetime on the plan. This lack of flexibility makes it difficult for a Medigap issuer to accept the administrative and financial risk of enhancing benefits. MA’s broad annual flexibility to include dental, vision, hearing, and wellness coverage gives MA a major competitive advantage. However, recent studies hint that the actual financial and health value of these enhancements may be small and these enhancements may be at risk going forward due to new financial pressures on MA plans.8
Individuals continuing to choose to supplement Medicare with Medigap generally do so in order to readily choose and change their providers; retain provider access flexibility when in different geographic locations throughout the year (snowbirds, for example); and cover their major health care needs without MA’s utilization reviews and the risk of prior authorizations denials.9 According to one study, more than 35 million prior authorization requests were submitted to MA plans in 2021, with 6% initially denied, hinting at barriers and complexities as well as likely delays in receiving necessary care.10
Providers may also appreciate Medigap-covered patients over MA patients, as the Medicare fee schedule is often more advantageous than that of MA,11 and there is little to no red tape surrounding prior authorization and concurrent/retrospective review. Recently, several providers have started campaigns to influence patients’ Medicare coverage decisions or decided not to take certain MA plans at all.12 Given the greatly increasing degree of health care providers’ services that will shift to Medicare patients in the coming decade, and thus the importance that payments from traditional Medicare and MA plans have on providers’ finances, these campaigns will likely grow in the coming years. Unlike the typical case for health insurers, health care providers’ finances were typically negatively affected by the pandemic, and many of them are still in recovery mode.
Guarantee Issue: A Competitive Difference but an Emerging Political Risk
Across the country, MA plans have a consistent annual open enrollment period where Medicare enrollees can change carriers and plans without having to worry that an insurance company may not accept them due to their age or health status. Similar open enrollment consistency does not exist in the Medigap market. Two states, Connecticut and New York, provide Medicare enrollees with year-round Medigap guarantee issue rights. A handful of states have some annual open enrollment window where an enrollee may switch Medigap carriers (but perhaps not be able to switch plan choice). When available, these windows often do not align with MA’s open enrollment timing and are often not consistent within the state. For example, some are based on the enrollees’ birthdates (California, Idaho, Illinois, Nevada, and Oregon); the policy anniversary (Missouri); a timing selected by the carrier (Maine); or a fixed period that is consistent for all Medigap carriers (Massachusetts and, recently, Minnesota).13 In the remainder of states, Medigap tends to be a “sticky” product selection, because if seniors leave their Medigap carrier, there are no guarantees they can return to that carrier at a later date. Given that people tend to be less healthy as they age past 65, leaving a Medigap carrier is a very risky choice in most states.
Due to complaints from seniors to state legislators, there is a growing regulatory risk to Medigap insurers coming from the broadening of guarantee issue rights, which attempts to make the opportunities to change Medigap carriers similar to those that exist in the MA market. While consistency in attracting new enrollees offers growth opportunities to Medigap insurers and is in some ways always an election for a Medigap insurer willing to take all comers, this change comes with a lot of underwriting risk. Most insurers rely on the sticky nature of Medigap to help in understanding their claims risks, which helps to obtain state approval for Medigap rate increases. Upheaval of the eligibility rules comes with a high risk for unexpected losses. While MA plans have federal risk mitigation programs that help MA insurers deal with this particular underwriting risk (called risk adjustment), such protections do not exist in the Medigap market. Combined with other federal and state political risks, such as the potential for new benefit mandates or design requirements, political risk is certainly on the watch list for the Medigap industry.
Reinsurance for Medicare Plans
Reinsurers make excess-of-loss reinsurance available for Medigap plans, though such reinsurance is not commonly sought. The fundamental homogeneity of the Medigap population, the product’s tie-in to the traditional Medicare fee schedule, and the supplementary nature of the coverage has made Medigap a relatively predictable coverage for insurers to offer.
In contrast, excess-of-loss reinsurance is commonly sought by MA plans, as MA insurers are at risk for traditional Medicare’s share of the cost, which has a much higher risk for hospitalization cost outliers, and further because MA payers are not required to directly reference Medicare’s fee schedule in their provider contracts. While this often implies in practice that MA plans are paying providers less than the traditional Medicare fee schedule would have paid on an overall basis, the disconnect from the Medicare fee schedule subjects MA providers to more risk for outlier claims.
That being said, material risks are emerging for Medigap insurers for which reinsurance could help, particularly including the high-cost specialty drugs14 covered in Part B and the growing number and type of gene and cell therapies. Medigap insurers are also experiencing risk in obtaining necessary rate increases from state regulators over time. State regulators are particularly sensitive to the rate increases affecting this population, given that most Medigap enrollees are on a fixed income. Reinsurers often provide their customers with free or low-cost research and experience studies that often can help to demonstrate the relevance for the emerging risks and the need for rate increases. Some reinsurers also provide capital-motivated reinsurance, which can help relieve some of the capital strain that relatively rapid growth can place on insurers.
Why Is Medigap “Homogeneous”?
Medigap is relatively more homogenous than other health plan types due to the following:
- With few exceptions, the policies are for one person at a time.
- The plan design choices of the policies are consistent in the vast majority of states.
- Each enrollee has the same Medicare plan underlying the policy, which pays for a large share of health care costs.
- Over time, most Medigap enrollees stay with the same policy/carrier from which they first purchased their policy.
- Purchasers tend to be wealthy enough to be willing to pay additional premiums to cover more than what the traditional Medicare program provides.
- Most Medigap enrollees are over age 65 and experience similar aged-related health conditions.
Some Final Thoughts
The Medigap, MA and Part D markets provide a great deal of choice – choices so numerous that they can create a lot of stress for consumers and providers alike. After a session at last year’s SOA Impact conference, one of the questions posed to the panel of health actuaries was, “Which type of Medicare plan (MA versus Medigap) would each of you choose, and why?” Our answers were surprising, but rather than me telling you why, I suggest that you pose this question to your peers and let me know what you find out.
At RGA, we are eager to engage with clients to better understand and tackle the industry’s most pressing challenges together. Contact us to discuss and to learn more about RGA's capabilities, resources, and solutions.
This article was originally published in the Society of Actuaries' March 2024 issue of the Health Watch newsletter.