Gestational diabetes mellitus (GDM) is a condition in which maternal hyperglycemia develops during pregnancy and usually resolves post-partum
It is one of the most common endocrinopathies in pregnancy and its global prevalence is on the rise. In most cases, hyperglycemia in pregnancy is due to impaired glucose tolerance resulting from pancreatic beta-cell dysfunction and chronic insulin resistance.
GDM is associated with maternal morbidity and fetal mortality if left untreated, with consequences that can include increased risk of future cardiovascular disease (CVD) and type 2 diabetes mellitus (T2DM) in the mother and macrosomia and birth complications in the infant. Although the immediate impact of GDM may be very minimal on maternal mortality, there can be significant long-term consequences. Screening and appropriate management of GDM are therefore of the utmost importance for the health of both mother and child.
Introduction
Gestational diabetes mellitus (GDM) is a common complication of pregnancy in which women without previously diagnosed diabetes develop chronic hyperglycemia during gestation. GDM can occur at any stage of pregnancy but is more common in the second or third trimester.1 This definition applies whether insulin and/or diet modification is used for treatment, and whether or not the condition persists after pregnancy. It also does not exclude the possibility that unrecognized glucose intolerance may have preceded or begun concomitantly with the pregnancy.2
Epidemiology and Risk Factors
Worldwide prevalence estimates for GDM are difficult to interpret due to inconsistency in its screening and diagnosis.
The prevalence of high blood glucose (i.e., hyperglycemia) in pregnancy is known to increase rapidly with maternal age. In 2019, it was estimated that globally, one of every six mothers who gave birth to a live infant (20 million) had experienced some form of hyperglycemia in pregnancy, of which an estimated 84% of the cases were GDM. Currently, approximately 10% to 15% of all pregnancies are complicated by GDM, with the highest prevalence seen in Southeast Asia at around 27%.3
The ongoing obesity epidemic, coupled with rising maternal ages and sedentary lifestyles, are also major contributors to the global increase in GDM. Most cases of hyperglycemia in pregnancy are in low-and middle- income countries, where access to maternal care is limited.4
Any woman can develop GDM during pregnancy, but the risk is higher if certain maternal factors exist, such as: obesity before pregnancy or excessive gestational weight gain; advanced maternal age; presence of diseases of insulin resistance (e.g., polycystic ovarian syndrome [PCOS]); a personal history of chronic hypertension and/or of low or high birth weight babies; a family history of insulin resistance or any form of diabetes; ethnicity (prevalence rates are known to be higher in Black, Hispanic, Native American and Asian women);5 and genetic polymorphisms.
Signs, Symptoms, and Prognosis
Diagnosis of GDM is often through prenatal screening rather than through reported symptoms. However, symptoms such as polydipsia, polyuria, dry mouth, or fatigue may develop with poorly controlled maternal blood sugar levels.6
GDM risk is higher if certain maternal factors exist.
GDM is associated with multiple short-term adverse maternal and perinatal outcomes and is known to have long-term adverse health effects on the mother and child.7
During pregnancy, short-term risks include spontaneous abortion, premature birth of the fetus, and stillbirth. GDM may also be associated with fetal anomalies and complications such as macrosomia, shoulder dystocia, neonatal hypoglycemia, or hyperbilirubinemia. Neonatal respiratory distress syndrome is commonly seen as well.
Operative delivery (caesarean section or instrumental assist) is frequently needed and may also be necessitated by maternal factors such as pre-eclampsia or gestational hypertension. Antenatal depression is also frequently experienced by GDM mothers.
Post-pregnancy, GDM can be an indicator of future diabetes and cardiovascular disease (CVD).8 Long-term maternal risks associated with GDM include:
Impaired glucose tolerance. Approximately 30% of women with GDM experience impaired glucose tolerance during the early postpartum period.
Metabolic syndrome. Approximately one-third of women with mild GDM (i.e., one normal fasting glucose during an oral glucose tolerance test [OGTT]) develop metabolic syndrome within five to 10 years of delivery.
Type 2 diabetes mellitus (T2DM). GDM is often indicative of underlying maternal pancreatic beta- cell dysfunction, which increases maternal risk of development of T2DM.9 According to a 2018 study, approximately 60% of women with a history of GDM develop T2DM later in life. The yearly risk of conversion to T2DM is approximately 2% to 3%.1 A more recent study noted that for women with GDM, longer duration of lactation was associated with a lower risk of T2DM and a favorable glucose metabolic biomarker profile.10
Cardiovascular disease. Women with GDM are at higher risk of not only developing CVD, but of also developing it at a younger age than women with no history of GDM. Some studies suggest that GDM permanently alters female vasculature, causing increased CVD risk. A recent study also reported increased risk of CVD and lower HDL levels among women with a history of GDM.11
Recurrence. GDM usually resolves post-delivery, but there is a high risk of recurrence in subsequent pregnancies. Recurrence is seen more among advanced age pregnant women and among women who gain more weight between their pregnancies. Approximately one-third to two-thirds of women with GDM will have GDM in subsequent pregnancies. Women who had GDM also have a threefold risk of developing T2DM with each additional pregnancy compared to women without additional pregnancies.8
There are also hazards for children born to mothers with GDM. These children are at increased risk for obesity, T2DM, CVD, and associated metabolic diseases. In some of these children, impaired glucose tolerance can first be noticed at a very young age. GDM in mothers could also establish a propensity for GDM in their female children, who may be more likely to experience it in their own future pregnancies.1
Investigation and Diagnosis
There is currently not just a lack of uniform strategy for screening GDM, but also an absence of an accepted, evidenced-based, gold standard for diagnosis of GDM during routine antenatal screenings.
The clinical criteria often applied are from the World Health Organization (WHO), the American Diabetes Association (ADA), the International Association of Diabetes in Pregnancy Study Groups (IADPSG), the American College of Obstetricians and Gynecologists (ACOG), and the Canadian Diabetes Association (CDA).
WHO, for example, recommends that a diagnosis of GDM be made when one or more of the following metrics are found:
Fasting glucose of >126 mg/dL (7.0 mmol/L)
Two-hour plasma glucose of >200 mg/dL (11.1 mmol/L) following a 75-gram oral glucose load
Random blood glucose of >200 mg/dL (11.1 mmol/L) in the presence of diabetes symptoms12
The American Diabetes Association (ADA), meanwhile, recommends the use of either a one- or two-step screening approach at 24 to 28 weeks of gestation in pregnant women not previously known to have diabetes.2
Table 1: ADA Screening Approach for GDM |
75 gm OGTT* | 100 gm OGTT* ** |
A diagnosis of GDM can be made when any of the following three plasma glucose levels are met or exceeded: Fasting: 92 mg/dL (5.1 mmol/L) 1 hour: 180 mg/dL (10.0 mmol/L) 2 hours: 153 mg/dL (8.5 mmol/L)
| A diagnosis of GDM can be made if at least two of the following four plasma glucose levels are met or exceeded: Fasting: 95 mg/dL (5.3 mmol/L) 1 hour: 180 mg/dL (10.0 mmol/L) 2 hours: 155 mg/dL (8.6 mmol/L) 3 hours: 140 mg/dL (7.8 mmol/L)
|
*Oral Glucose Tolerance Test
**This test is performed after failing an initial screening with a 50-gm glucose challenge.
GDM Management
Several treatments and healthcare practices can reduce the risks GDM can pose to pregnancy.
- Lifestyle changes are the first approaches recommended for management of GDM. Changes in diet and exercise habits are essential components of lifestyle change and may suffice for treatment of about 70% of those experiencing GDM. The changes should aim to limit the gestational weight gain and improve glycemic control.13
- Monitoring certain metrics can be beneficial. GDM patients are encouraged to monitor their blood glucose levels four-times per day, preferably prior to meals, as the risk of fetal macrosomia rises with increased maternal blood glucose following meals. Measuring glycosylated hemoglobin (HbA1C) can have some benefit, but due to the increase in red blood cell mass and turnover during pregnancy, frequent measurements of it might not be useful. However, in women with an initial HbA1C of more than 6.5%, regular assessments (one every three months) might be helpful.14
- Insulin is preferred for treating GDM as it does not cross the placenta to a measurable extent.15 The type and timing of insulin doses depends on the blood glucose levels.
- Pharmacotherapy is the next line of treatment, but needs to be done with great care, as all oral agents lack long-term safety data.16, 17, 18 Metformin and glyburide are not advised as first-line agents, as both cross the placenta to the fetus, but they are occasionally prescribed.
- Post-partum screening every three years to check for development of diabetes or prediabetes should be lifelong for women with a history of GDM.19
Insurance Implications
GDM and T2DM
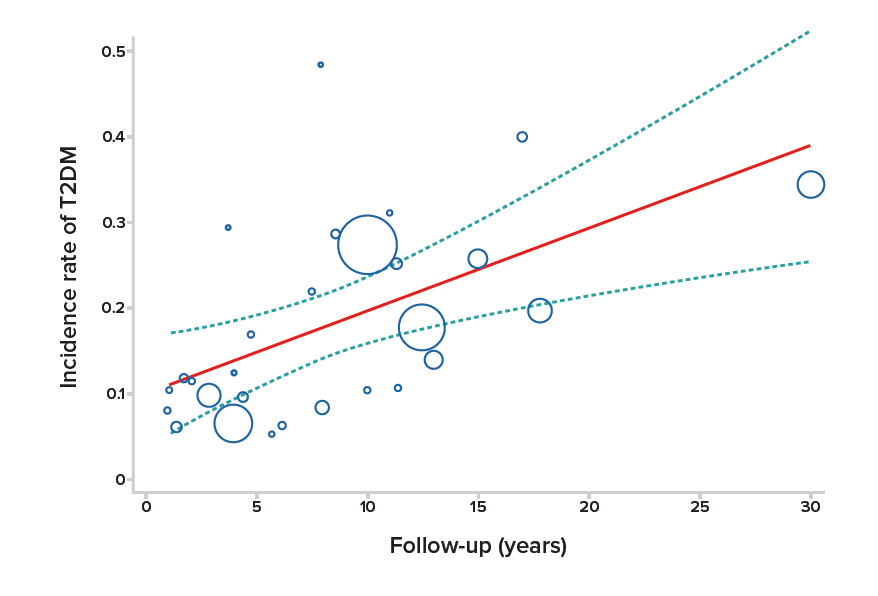
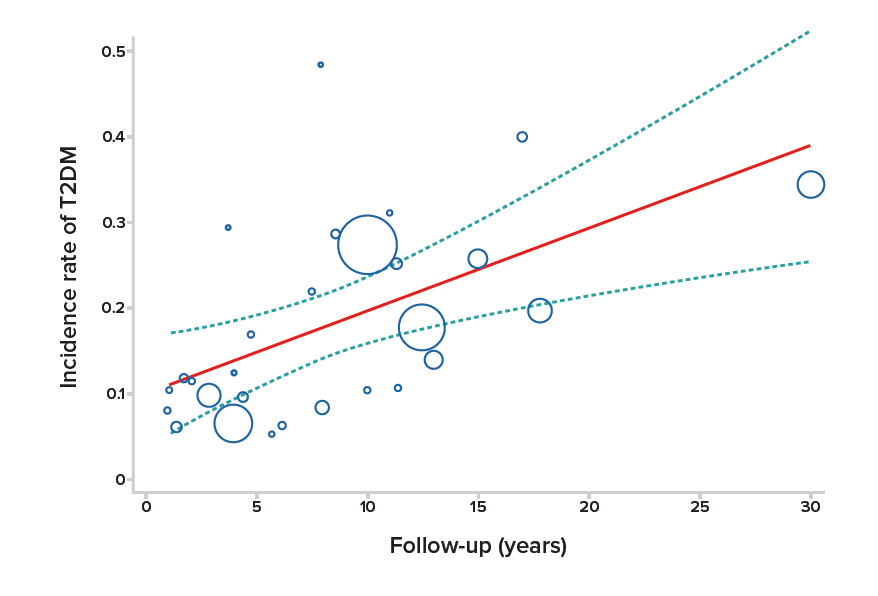
In 2020, two meta-analyses were conducted. The first analyzed 20 studies containing a total of 1,332,737 participants and noted that the pooled relative risk (RR) of developing T2DM was almost 10 times higher among women with GDM than among the controls.20 The second, in which 170,139 women with GDM participated, reported that the incidence rate of developing T2DM after GDM was approximately 26%. It also noted that the development of T2DM after GDM increased an estimated 9.6% per year of follow-up.21 (See Figure 1, below)
Figure 1:
Incidence of T2DM Among Women with GDM Over Time21
A 2018 study investigated the impact of GDM on long-term T2DM risk among women at different time periods post-partum. Findings indicated that the relative risk of developing T2DM was highest at three to six years after GDM and for women under 40 years of age.
This study also found that previous GDM was associated with a 7.76-fold risk of developing T2DM and that women with early-onset T2DM (under age 40) were at higher risk of experiencing diabetes as well as cardiovascular and microvascular complications than those with later-onset T2DM. Finally, Asian women, as well as women of advanced-maternal age and women with higher body mass indexes (BMI >30.0 kg/m2), were found to be at higher risk of developing T2DM.22
GDM and CVD
There is a distinct relationship between GDM and future risk of CVD. Women who had GDM have been found to be at more than twice the risk of future cardiovascular events during follow-up than women without GDM.23 GDM is also associated with increased risk of myocardial infarction (MI), with a fully adjusted hazard ratio of 1.45 (95% CI; 1.05-1.99).24
GDM and Cancer
Diabetic individuals overall are known to be at higher risk of certain types of cancers. Women with GDM have been found to have a higher risk of developing cancers than women without GDM (2.24% vs 1.96%). Hence, regular cancer screening is warranted for women who have had GDM.25
GDM and Maternal Insurance Benefits
For maternal coverage products, it should be kept in mind that the cost of healthcare will be higher for pregnant women with GDM. The additional costs include GDM diagnosis and treatment, maternal complications, neonatal complications, and increased need for assisted deliveries. The cost of outpatient expenses will also be higher, as they may need to include additional physician visits, GDM screening, diet and exercise consulting, medical tests, drugs, and insulin.
Conclusion
The global burden of GDM has been on the rise with increases in obesity and changes to lifestyle. There is a well-established association between increasing hyperglycemia in pregnant women and the occurrence of adverse maternal and fetal outcomes. Women with GDM are at an increased risk of complications during pregnancy and at delivery. However, the risks can be reduced if the condition is detected early and managed effectively.
The impact of GDM may be very minimal on immediate mortality, but it may have significant long-term consequences for the health and well-being of the individual with GDM. For insurance purposes, it is important to consider the history, complications, and long-term outcomes of GDM on maternal morbidity, fetal mortality, and that it may be a precursor for increased risk of diabetes, CVD, and cancers.